The Onset and Duration of Action of 0.2% Lidocaine in a One-per-Mil Tumescent Solution for Hand Surgery
Article information
Abstract
Background
One-per-mil tumescent solution, which contains 0.2% lidocaine with 1:1,000,000 epinephrine, has been reported to be clinically effective for hand surgery under local anesthesia. However, it was lacking in its basic pharmacokinetics profile in regard to the onset of action (OOA) and duration of action (DOA).
Methods
A randomized, double-blind study was conducted on 12 volunteers who met the inclusion criteria from October to November 2014. All volunteers had their right and left ring finger pulps injected with either one-per-mil solution or 2% lidocaine. Semmes-Weinstein and two-point discrimination tests were used to test sensation. Visual analogue scale was recorded at the time when the finger lost its sensation and when it regained normal sensation to measure the OOA and DOA. The data were then analyzed with a paired t-test and a Wilcoxon signed-rank test.
Results
The OOA and DOA of 2% plain lidocaine were 1 minute and 99.67 minutes, respectively. Meanwhile, 0.2% lidocaine in a one-per-mil tumescent solution showed an OOA of 5 minutes and a DOA of 186.83 minutes. The OOA of 0.2% lidocaine in a one-per-mil tumescent solution is statistically shorter than 2% plain lidocaine (P=0.04); while its DOA is statistically longer than 2% plain lidocaine (P<0.001).
Conclusions
The 0.2% lidocaine in a one-per-mil tumescent solution is statistically and clinically superior to 2% plain lidocaine in achieving longer duration of local anesthesia.
INTRODUCTION
Local anesthesia has been frequently used in many hand procedures such as fingertip injuries, laceration repair, repair of tendon rupture, dislocation reduction, foreign body removal and wound debridement, and tumor excision [123]. The ideal local anesthesia agent should be able to provide a relatively long duration of anesthesia, which allows surgeons to accomplish complex surgical procedures, and provides a long period of postoperative pain relief for the patient [24].
For many years, lidocaine has been safely used as a local anesthetic agent [5]. Meanwhile, the use of lidocaine with epinephrine has gained popularity in the field of hand surgery [2467]. The epinephrine concentration used in a tumescent solution is within the range of 1:80,000 to 1:400,000 [8]. Multiple reviews and clinical series have shown that epinephrine is safe to be used in the digits, as no cases of finger necrosis have been reported [9101112].
In regard to the onset and duration of action (DOA) of lidocaine in a tumescent solution, only limited data are available. According to Keramidas and Rodopoulou [8], the onset of action (OOA) of 2% lidocaine was 1.3 minutes. As for the DOA, a study by Thomson and Lalonde [2] reveals the DOA of 2% lidocaine and 2% lidocaine with 1:100,000 epinephrine was 4.9 hours and 10.4 hours, respectively.
The most recent practice of tumescent technique in hand surgery has been to use a one-per-mil solution (1:1,000,000 epinephrine with 0.2% lidocaine) [13]. Further reports have shown the effectiveness of a one-per-mil tumescent solution in facilitating hand surgery without a tourniquet. Interestingly, these reports have also shown the ability of 0.2% lidocaine (in a 1:1,000,000 epinephrine solution) to provide adequate anesthetic effect in hand surgery under local anesthesia [614]. However, the onset and DOA of 0.2% lidocaine with 1:1,000,000 epinephrine has not been reported with confidence. Thus, we aimed to study the onset and DOA of 0.2% lidocaine in a one-per-mil tumescent solution for use in hand surgery, and also to compare it with 2% lidocaine without epinephrine, which is the most widely used agent for local anesthesia.
METHODS
A randomized, double-blind, matched-pair study was conducted to measure the onset and DOA of 0.2% lidocaine in a one-per-mil solution as well as a 2% plain lidocaine solution injected in healthy subjects with the tumescent technique, from October to November 2014, at our institution. This study conformed to the principles outlined in the Declaration of Helsinki and received approval from our Institutional Review Board.
Twelve subjects were enrolled based on the simplified formula for difference in means with assumed difference 4, standard deviation 5.4, statistical power 90%, and type I error 5%. The subjects were healthy males, aged between 18 to 30 years old, who voluntarily joined this study and met the inclusion criteria. Body mass index (BMI) criteria ranged from 18.5 to 23 kg/m2. Female volunteers, or male volunteers with detectable scars on any of the ring fingers or with a history of heavy smoking, blood or coagulation disorder, neurovasculopathy, liver and renal disease, or an allergy to lidocaine, were excluded. These subjects were selected using a convenient sampling method. Subjects who were not able to comply with the study protocol were excluded.
The volume of the subjects' hands were measured. Each subject was asked to dip his hand slowly into a volumetric flask filled with pre-measured water until the water reached the distal wrist crease, which was considered the level of the subject's wrist. The water that overflowed spilled into a bowl that was placed beneath the volumetric flask. The difference in water volume inside the flask before and after hand dipping reflected the volume of the subject's hand.
A single researcher (the first author) performed the injection into the ring fingers of both hands for all of the subjects. Another single researcher (the second author) conducted the measurement and assessment. Each subject was entrusted with one randomized envelope that contained information regarding which of the subject's ring fingers received the 2% lidocaine solution without epinephrine (the control group) and which ring finger received the 0.2% lidocaine in a one-per-mil tumescent solution (the study group). Neither the subjects and nor the researchers knew the contents of the envelopes containing the solution labels, which were prepared by another person who performed the randomization.
Pain sensation of the ring finger pulp was tested using a red monofilament sized 4.56 with 4 grams pressure force taken from the Semmes-Weinstein (SW) monofilament test (Stoelting Co., Wood Dale, IL, USA) and two-point discriminator (Stoelting Co.) which was set at 3 mm. Both tests were performed 5 minutes before injection. The subject was asked to rate his pain level by marking the visual analogue scale (VAS) chart accordingly to measure the baseline VAS score.
The senior author injected a different solution into each ring finger without knowing which type of solution it was. The solution was injected slowly into the subject's ring finger pulp on each hand, until the pulp turned pale. The same volume of solution was injected into the other ring finger of the same person on the next day.
Every subject was asked about the physical feeling of his finger after the injection. The pain level was recorded every minute until the sensation of the pulp was lost by using the SW monofilament and two-point discriminator (2PD) to determine the OOA of lidocaine in both solutions.
The subject was kept for monitoring and asked every 30 minutes about the pain sensation in his finger pulp by using the SW monofilament and 2PD, until the subject regained sensation. Besides being tested with instruments, the subject was also asked to actively stop the monitoring stopwatch when sensation returned. Subsequently, the timing was recorded to determine the length of DOA time. At this time, the subject was asked to rate his level of pain and give a mark on the VAS chart.
The subjects were then monitored for the subsequent 2 hours, to detect any early complication. They were also provided with 4 tablets of paracetamol (500 mg) to be consumed, to ease the pain during the first day in case they felt it. In case of prolonged pain after 24 hours, the subject was instructed to contact the researchers for further examination. A summary of the study procedures is shown in Fig. 1.
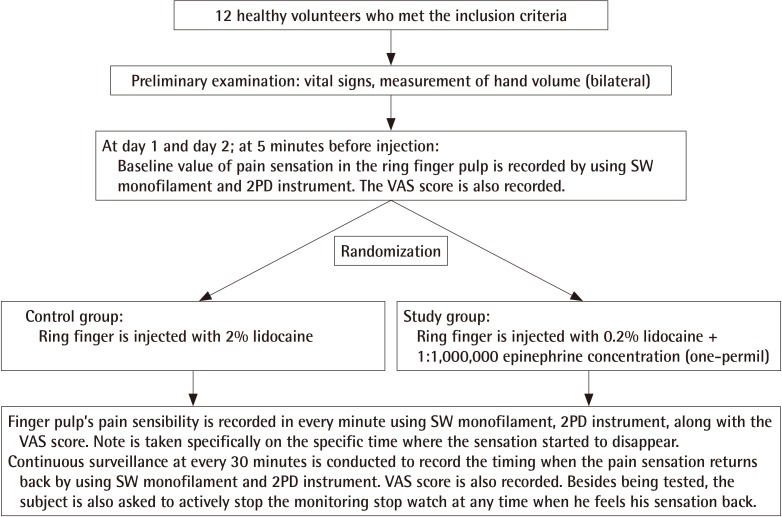
Research algorithm
Subjects are randomly classified into two groups. The ring finger is injected with a one-per-mil tumescent solution in the study group, whereas the finger in the control group is injected with 2% pure lidocaine. 2PD, two point discriminator; SW, Semmes-Weinstein; VAS, visual analogue scale.
IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) was used to process the data, which was then presented in descriptive form as the mean and standard deviation for numerical data with a normal distribution, and the median with minimum and maximum points for numerical data with an abnormal distribution. A paired t-test was used to analyze the normally distributed data, while a Wilcoxon signed-rank test was used for abnormally distributed data. The significance level was set to P<0.05.
RESULTS
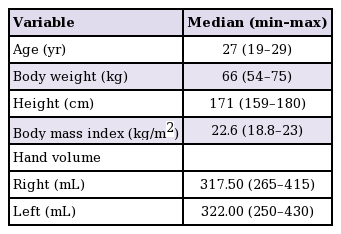
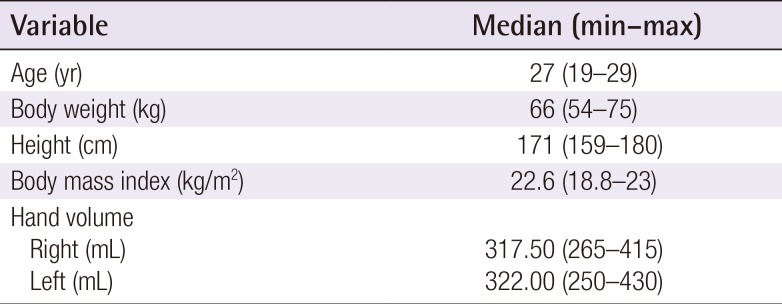
Twelve eligible volunteers participated in this study. All subjects were male, with an average age of 27 years, ranging from 19 to 29 years old, and the average BMI was 22.6, ranging from 18.8 to 23. The average volume of the subjects' right hands was 317.50 mL (range, 265–415 mL), while the average volume of the left hands was 322.00 mL (range, 250–430 mL). There was no significant difference between the right and left hands (P-value>0.05). The demographic characteristics of the subjects are detailed in Table 1.
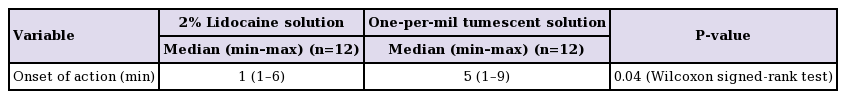
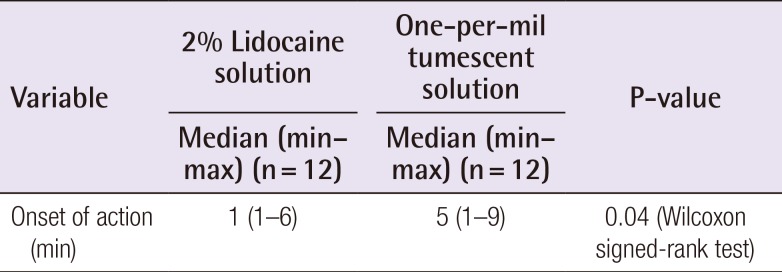
Table 2 shows the onset of action (OOA) for both groups. In the 2% lidocaine group, the median OOA time was 1 minute, ranging from 1 to 6 minutes. Out of 12 subjects, there were 10 subjects who experienced loss of sensation within the first minute. Meanwhile, the two other subjects experienced loss of sensation in 2 and 6 minutes. On the other hand, in the one-per-mil tumescent solution group, the OOA was much more varied, with a median value of 5 minutes (range, 1–9 minutes). Both groups were analyzed statistically and found to differ with statistical significance (P=0.04; Wilcoxon signed-rank test).
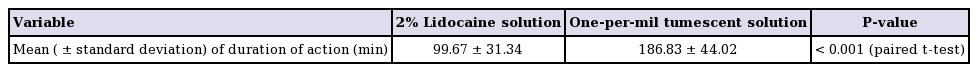
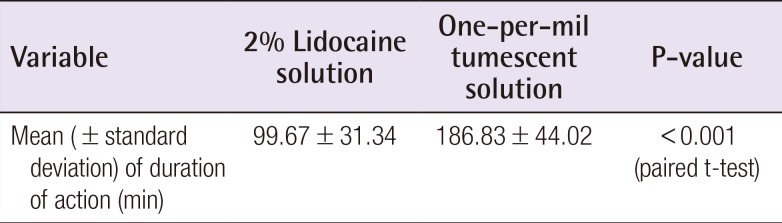
As shown in Table 3, the DOA of the 2% lidocaine group (99.67±31.34) was shorter than the DOA of the one-per-mil tumescent solution group (186.83±44.02). This difference was found to be statistically significant (P<0.001; paired t-test).
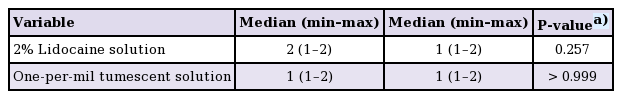
Table 4 shows no significant difference between the baseline sensibility and the sensibility at the end of DOA in both the 2% lidocaine group (P=0.257) and the one-per-mil tumescent solution group (P>0.999). The score ranged between 1 and 2 in both VAS at 5 minutes before injection and at the end of DOA in both groups.
DISCUSSION
Most surgeons agree that the ideal local anesthetic agent should provide a relatively long DOA to accommodate the completion of the surgical procedure, whether in an emergency or an elective setting, especially for complex cases [2]. In order to achieve longer duration of action, epinephrine is added to local anesthetic agents, such as lidocaine [2467]. Moreover, since Lalonde introduced the wide–awake local anesthesia no tourniquet (WALANT) technique using lidocaine in the last decade, many surgeries for the hand and digit have been performed with this technique [915161718], where epinephrine is used to provide a tourniquet effect.
Epinephrine plays a role in the vasoconstriction of the blood vessels, which provides hypoperfusion [2], without necessarily causing ischemia [19]. Prolonged DOA of lidocaine in a one-per-mil tumescent solution or in any concentration of epinephrine is caused by the delayed absorption of lidocaine while the blood vessels in the tissue are being constricted. Moreover, the increased tissue hydrostatic pressure resulting from the tumescent injection technique has been identified as a factor that may contribute to the slow absorption of lidocaine [20].
Until recently, a pneumatic tourniquet has been considered mandatory in providing a bloodless operative field in hand and upper extremity surgery, but it is undeniable that the application of this device is not without risks. The use of a tourniquet may result in complications to the muscle, nerve and skin, compartment syndrome, and other systemic effects [21]. Post-tourniquet syndrome involves edema, stiffness, and weakness of the limb [21]. Those problems are caused by the ischemic injury and edema after reperfusion [2122]. Other disadvantages of the pneumatic tourniquet are that the patient must be treated under general or regional anesthesia to avoid pain. In addition, the tourniquet can only be applied for about 1.5–2 hours [2122]. Therefore, the addition of epinephrine to a local anesthetic solution has its own merits. Not only does epinephrine prolong the DOA of lidocaine, it also allows us to achieve a clear and bloodless operative field that is comparable to what could be achieved with tourniquet application in a fully conscious patient, without the time limitation and without the fear of post-tourniquet complications [2615].
This study revealed that the OOA of 2% lidocaine was 1 minute (ranging from 1 to 6 minutes). This result was in accordance with the study by Keramidas and Rodopoulou [8], who showed that 2% lidocaine has rapid OOA. In this case, it was 1.3 minutes (ranging from 1 to 2.7 minutes). In a systematic review performed by Vinycomb and Sahhar [23], it was revealed that the mean OOA of 2% lidocaine was 3.1 minutes.
The DOA of 2% lidocaine in our study was 99.67±31.34 minutes. This is very short when compared to the reported DOA of 2% lidocaine by Thomson and Lalonde [2], which was 4.9 hours. However, their measurement method is merely subjective. In their study, subjects recorded the time when their fingers had completely regained normal sensation. Although other sensations such as touch and pressure come back later than pain sensation, it is the pain sensation that we studied in relation to our needs in surgery. Thus, their study would be more convincing if the subjects had been tested for pain sensation to measure the DOA, as we did in our study. Moreover, they performed a "digital tumescent block" instead of a "purely local infiltration by tumescent technique," as we did in the subjects' finger pulps. Their "digital tumescent block" was performed with injection into the volar side of the proximal phalanx just near the digitopalmar crease. This might explain the difference between our results and the results of their study. Another study by Vinycomb and Sahhar [23] showed through a systematic review that the mean DOA of 2% lidocaine was 2 hours. However, they stated that all studies included in their review were of moderate to very low quality of evidence.
Regarding the 0.2% lidocaine in a one-per-mil tumescent solution, the OOA from our study was 4.67±2.53 minutes after injection, while Oliveira et al. [24] showed in their study on the buccal and palatal tissue that the OOA of 2% lidocaine mixed with a 1:100,000 concentration of epinephrine was 3 minutes (ranging from 1 to 7 minutes). Although anatomical region plays a role in providing different results, both hand and intra-oral surgeries are similar in that both deal with highly vascularized tissue and structures. Obviously, the slower OOA of 0.2% lidocaine in a one-per-mil tumescent solution compared to the OOA of 2% lidocaine mixed with a 1:100,000 concentration of epinephrine may be caused by the 10 times lower concentration of both lidocaine and epinephrine. However, the difference between the two study outcomes is not important clinically.
As for the DOA of 0.2% lidocaine in a one-per-mil tumescent solution based on the pain test using SW monofilament, we found a result of 186.83±44.02 minutes. Interestingly, Prasetyono et al. [14], who performed surgeries using the same one-per-mil tumescent solution as a local anesthetic agent, revealed successful procedure completion of up to 270 minutes. Even though the DOA of 2% lidocaine mixed with a 1:100,000 concentration of epinephrine in the study by Thomson and Lalonde [2] was 10.4 hours, the results came as reports by the subjects who were given "digital tumescent block" anesthesia without experienced-pain testing, as we have explained previously. Moreover, both the lidocaine and the epinephrine concentration used in their study was 10 times higher than what we used with the one-per-mil solution. On the other hand, the DOA of 2% lidocaine mixed with a 1:100,000 concentration of epinephrine in the study by Oliveira et al. [24] was 227.5 minutes (ranging from 159 to 273 minutes), which is closer to our result, as they also determined the end of the duration of lidocaine and the return to normal sensation by giving a pain stimulus (in their case, using a pulp tester for the tooth). Although it has yet to be proven through a direct comparative study, this shows that 0.2% lidocaine added to a 1:1,000,000 concentration of epinephrine can be compared to 2% lidocaine in 1:100,000.
Vinycomb and Sahhar [23] found the OOA and DOA of lidocaine mixed with epinephrine was 3.5 minutes and 5 hours respectively. Unfortunately they did not mention the concentration of lidocaine or epinephrine in the solution, thus making it difficult for us to make a comparison.
SW red monofilament sized 4.56 with 4 grams pressure force and a 2PD instrument were used to confirm whether the subject experienced pain that as expressed by VAS score. Although the actual purpose of the SW test and 2PD test are to evaluate pressure perception and tactile sensation, respectively [25], we found that both the 2PD test and the SW test using the red monofilament could actually induce mild pain sensation. By the time the effect of the lidocaine wore off, the subject would start to regain their pain sensation and sensibility. The subjects would then express the pain by pointing to the VAS, which indicates the end of DOA. This might be the reason why the DOA time of lidocaine in a one-per-mil tumescent solution is shorter compared to the references along with the reported clinical experiences of Prasetyono et al. [614]. Pain is undeniably a subjective matter; thus we value every VAS score expressed by the subjects in any case. However, as pain and sensations are subjective, this was also a limitation of the study, as we could not rule out such an uncontrollable factor. We could only trust the subjects and depend on their evaluation in determining both the OOA and the DOA of the anesthetic solution. This difficulty notwithstanding, the VAS score at the time before injection and after regaining sensibility proved to have no difference statistically. Therefore, we are sure that the VAS score recorded after the return of sensation represents the end of the DOA of lidocaine.
In sum, this study did not need to provide a comparative group to obtain data about the OOA and DOA of the one-per-mil tumescent solution. However, to make it more useful in regard to discussion of the kinetics, the authors compared it with lidocaine 2%, the commonly-used local anesthetic for rendering a finger numb, rather than presenting this study as a single cohort outcome. Furthermore, the aim of this study was not to identify the best epinephrine concentration to obtain the effect of an anesthetic agent in a certain concentration, nor was it to identify the best anesthetic agent with a certain concentration in a certain or in differential epinephrine concentration. This study was intended to provide specific data regarding the practice of using a one-per-mil solution that has been lacking in relation to basic pharmacokinetics. Comparing the one-per-mil tumescent solution with other regimens is another issue, which should be pursued through further studies.
In conclusion, the OOA of 0.2% lidocaine in a one-per-mil solution is statistically shorter than 2% plain lidocaine (4.67 minutes compared to 1 minute); however the DOA of 0.2% lidocaine in a one-per-mil solution is statistically, and more importantly, clinically longer than 2% plain lidocaine (186.83 and 99.67 minutes respectively). This result is remarkable given that 0.2% lidocaine is 10 times lower in concentration than the commonly used 2% plain lidocaine. Thus we can conclude that 0.2% lidocaine in a one-per-mil solution is clinically superior to 2% plain lidocaine in achieving longer duration of anesthesia.
Notes
No potential conflict of interest relevant to this article was reported.