Trichoblastic Carcinoma Arising from a Nevus Sebaceous
Article information
Nevus sebaceous is a hamartoma of the cutaneous structures that often presents at birth and typically involves the face and scalp. Nevus sebaceous is frequently complicated by the development of a variety of other benign or malignant neoplasms. The most frequently reported benign neoplasms are trichoblastoma and syringocystadenoma papilliferum. Malignant tumors are much less frequently observed in association with nevus sebaceous and include basal cell carcinoma, squamous cell carcinoma, sebaceous carcinoma, and others [1]. However, no previous reports have described trichoblastic carcinoma occurring secondarily to nevus sebaceous. We report a case of malignant trichoblastoma that arose from nevus sebaceous of the scalp in a 38-year-old woman.
A 38-year-old woman visited our clinic with a mass arising from a birthmark on the left parietal scalp. Six months prior to the visit, an erythematous mass had enlarged gradually in the plaque. Her chief complaints associated with the mass were itching, pain, and bleeding easily after small traumas. Physical examination of the scalp revealed a 5×2-cm yellowish, verrucous, hairless plaque, and a distinct 1.5×1.5-cm erythematous nodule was contained within it (Fig. 1). She had no personal or family history of underlying skin diseases or malignancies. A punch biopsy was done from the erythematous nodule, and showed that the mass was a malignant skin adnexal tumor. Therefore, she underwent complete surgical excision with 0.5 mm of normal skin surrounding the margins of the nevus sebaceous (Fig. 2). A frozen section biopsy showed that no tumor cells were present in the resection margin. The skin defect was then covered with a transpositional flap and primary closure was performed (Fig. 3). A histopathologic examination of the mass was performed, revealing the presence of a nodular tumor, which was diagnosed as trichoblastic carcinoma. It was composed of basaloid epithelial nests and strands. Some nodules showed central necrosis (Fig. 4). Nuclear atypia was present, as well as increased mitotic activity in a high-power view (Fig. 5).

Preoperative appearance. A papillary erythematous mass arose within a yellowish verrucous nevus sebaceous on the left parietal scalp.

A 4.7×1.8×0.4-cm oval, elevated lesion is seen, with an area of focal black pigmentation measuring 1.4×1.5 cm.
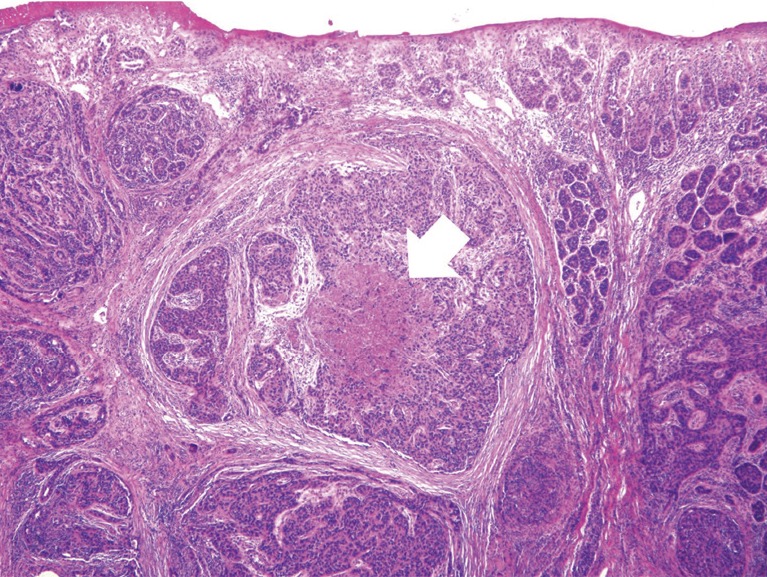
A low-power view reveals a vaguely nodular tumor. The tumor nodules were composed of variably sized nests of basaloid cells. Some tumor nodules had central necrosis (white arrow). Deep erosion was noted with loss of the epidermis (H&E, ×40).
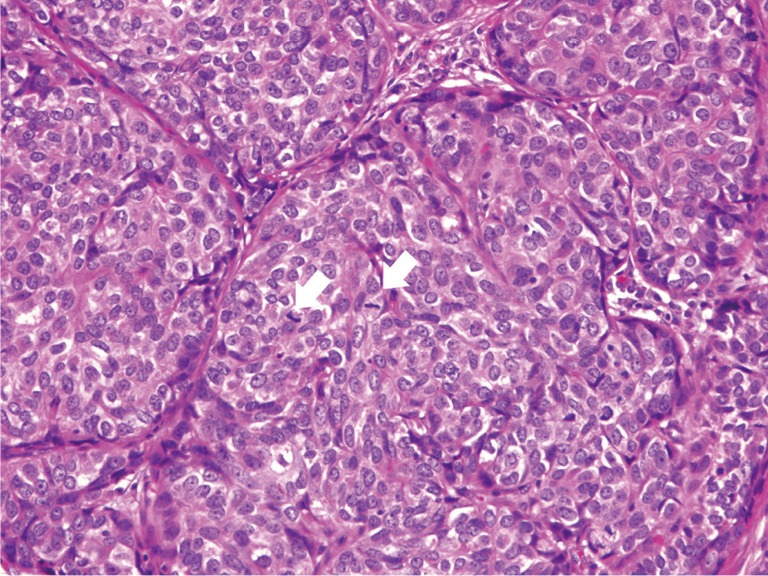
A high-power view shows atypical round to oval tumor cells. Many mitotic figures are visible (white arrows). Nuclear pleomorphism is present, with small nucleoli (H&E, ×200).
After confirming its malignancy, the patient was carefully evaluated for evidence of metastasis. A full body positron emission tomography-computed tomography (PET-CT) scan revealed no regional or distant metastasis. The patient is now under follow-up care.
Malignant trichoblastoma is a rare malignant adnexal tumor originating from the hair germ cells. Malignant changes in trichoblastoma may be related to its epithelial component (trichoblastic carcinoma), stromal component (trichoblastic sarcoma), or both (trichoblastic carcinosarcoma). Trichoblastic carcinoma usually presents on the scalp and face in middle-aged to elderly adults, who are often younger than patients with basal cell carcinoma. This patient was relatively young, at 38 years of age. According to the level of clinical malignancy, these tumors are divided into low-grade and high-grade lesions. Low grade trichoblastic carcinomas are characterized by the morphological aspects of trichoblastoma, but show infiltrative growth with the involvement of deeper tissues. They have also been referred to as aggressive trichoblastoma. They appear to grow slowly, with nodules or plaques occurring on the face that do not recur if completely removed. High-grade trichoblastic carcinomas have only been described recently, and are characterized by rapid enlargement with inflammation, a large size (>3 cm), necrosis, and a predilection for the trunk and extremities. They have the potential to exhibit aggressive clinical behavior and systemic spread, particularly to the lung [23]. A total of 13 cases of trichoblastic carcinoma have been reported in the literature, comprising seven low-grade and six high-grade carcinomas. Two patients with high-grade trichoblastic carcinomas are known to have died due to systemic progression of the disease [2].
All authors agree that surgery with complete removal is the treatment of choice. However, due to rarity of the disease, the optimal surgical margins have not yet been established. Ayhan et al. [3] reported a case of trichoblastic carcinoma in a 73-year-old woman. The tumor was excised with 0.5 mm of normal skin surrounding the margins, and the lesion was found to be a tumor with a free margin Cowen et al. [4] described a case of locally invasive trichoblastoma in which the tumor was excised in four stages using Mohs micrographic surgery. However, in this case, we performed wide excision with a safety margin of 0.5 mm surrounding the nevus sebaceous. The frozen section biopsy showed no tumor cells on the resection margin. Furthermore, PET-CT did not show metastasis. Over the course of 12 months of follow-up, our patient did not present with any signs of local or distant recurrence. We plan to observe her for the next five years. When surgical treatment is not possible due to unresectability of the cancer or because patients cannot undergo a reoperation after the first excision, radiotherapy may be considered as an adjuvant treatment [5].
We experienced a very rare case of trichoblastic carcinoma. Only 13 cases of malignant trichoblastic tumors have been reported in the literature. This is the only case of trichoblastic carcinoma that has been reported to occur in a nevus sebaceous. We obtained satisfactory treatment results using wide excision with a safety margin of 0.5 mm surrounding the nevus sebaceous, as verified by a frozen section biopsy. Herein, we report our case with a literature review.
Notes
No potential conflict of interest relevant to this article was reported.
