Acute Calcific Tendinitis in the Distal Interphalangeal Joint
Article information
Acute calcific tendinitis is a form of acute inflammation of the tendon, causing severe pain, swelling, and limited joint motion, and is characterized by radiologic evidence of periarticular calcification. The pathogenesis is not clear, but some believe that calcification may result from tendon hypoxia or a traumatic event [1]. Although it is a self-limited disease, in which periarticular calcification is eventually found to be resolved in radiologic imaging, it is often misdiagnosed, which can lead to unnecessary surgical intervention. It occurs most frequently in the shoulder and wrist, and least frequently in the hand, especially the phalanx [234]. We encountered a rare case of acute calcific tendinitis in a postmenopausal woman in the distal interphalangeal (DIP) joint and developed an appropriate management plan based on the correct diagnosis.
A 72-year-old female patient visited the emergency department due to severe pain in the left fourth finger that had developed three days previously. Simple radiography and ultrasonography were first performed, along with routine laboratory examinations, including C-reactive protein levels. A careful history was taken and a physical examination was then performed with the presumptive diagnosis of acute calcific tendinitis or gout, based on radiographic findings. The patient showed redness, swelling, and local heat and tenderness of the radial side of the DIP joint of the left fourth finger, but denied any history of trauma or other inflammatory disease.
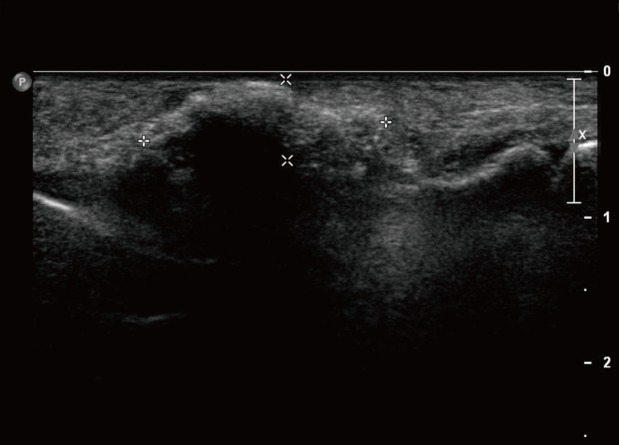
The patient's history revealed that she used the DIP joint extensively because of her occupation (operating a mill). The initial radiographs showed an ovoid calcification on the radial collateral ligament of the DIP joint of the left fourth finger (Fig. 1), and ultrasonography revealed ovoid hyperechoic calcification (Fig. 2). Her C-reactive protein level was elevated. Based on previous studies of the treatment of acute calcific tendinitis of other regions, an anesthetic agent (2% lidocaine, Huons Co., Seongnam, Korea) and a corticosteroid (Triam, Shinpoong Co., Seoul, Korea) were locally injected into the lesion [34]. Nonsteroidal anti-inflammatory drugs (NSAIDs) were administered to the patient, and a short arm splint was applied for immobilization. One day after conservative treatment, the symptoms were dramatically alleviated and simple radiographic findings showed that the appearance of the calcification had become mottled (Fig. 3), and the patient's C-reactive protein level decreased gradually. After one week of treatment, the patient experienced a complete resolution of pain and exhibited a full range of motion without difficulty. Follow-up radiographic findings after two months showed spontaneous resolution of the calcification (Fig. 4) [5].

The initial radiographs showed an ovoid calcification on the radial collateral ligament of the distal interphalangeal joint of the left fourth finger.

One day after conservative treatment was initiated, simple radiographic findings showed a change from an ovoid calcification to a mottled appearance, which co-occurred with the dramatic alleviation of the symptoms.

Follow-up radiographic findings after two months showed the spontaneous resolution of the calcification.
Acute calcific tendinitis of the DIP joint is a rare condition, and, to the best of our knowledge, has not previously been reported in this anatomical location. Careful attention to the history of the patient and simple radiography helped us to diagnose this case of acute calcific tendinitis correctly. Misdiagnosis of this disease can lead to unnecessary surgical treatment and delay symptom relief. Based on reports of this condition in other regions, such as the shoulder, elbow, and wrist, conservative management with NSAIDs and a local injection of an anesthetic agent and a corticosteroid were able to relieve the symptoms dramatically in our patient. In light of our experience, acute calcific tendinitis of the hand should be considered as part of the differential diagnosis of a painful finger joint.
Notes
This material was presented at the 71st International Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 1, 2013 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.