Multiple Epidermal Cysts in the Volar Skin of the Thumb
Article information
Epidermal cysts most commonly occur in hair-bearing areas, such as the scalp, face, neck, trunk, and scrotum, where many pilosebaceous glands are present [12]. Epidermal cysts do not commonly develop in the palmoplantar skin due to the absence of pilosebaceous glands. The etiology of epidermal cysts on the palms and soles may not involve inflammation of the hair follicle, but the traumatic implantation of epidermal elements [13]. In this report, we describe a case of multiple epidermal cysts that developed in the volar skin of the thumb.
A 53-year-old man visited our outpatient plastic surgery clinic, presenting with a slow-growing protruding mass on the left thumb (Fig. 1). He was a carpenter by occupation, and the mass developed after recurrent mechanical trauma by hammering for several decades. The 2.5×2-cm mass was located on the volar side of the distal phalanx of the left thumb. Upon physical examination, the mass was movable, without tenderness, redness, or a sense of warmth. We performed a simple X-ray of the hand to evaluate potential bony abnormalities and ultrasonography to determine the characteristics of the mass. The simple X-ray showed a normal bony appearance without bony erosion due to mass effect. We also found three subcutaneous low echoic masses on ultrasonography (Fig. 2). The overlying skin was incised horizontally and four masses were resected (Fig. 3). Mild adhesion was noted between the masses and the surrounding tissue, which was completely resected. The light microscopic examination of hematoxylin-eosin-stained sections was performed for all masses, which were diagnosed as epidermal cysts by a pathologist (Fig. 4). The wound was closed directly and followed up for two weeks. No complications, such as dehiscence, necrosis, hematoma, tingling sensation or hypoesthesia, or motility dysfunction occurred.

Three lobulated heterogeneous hypoechoic masses were seen on ultrasonography. The size of the largest mass was 1.3×0.6×1.2 cm and the other two small masses measured 0.5×0.5 cm each.
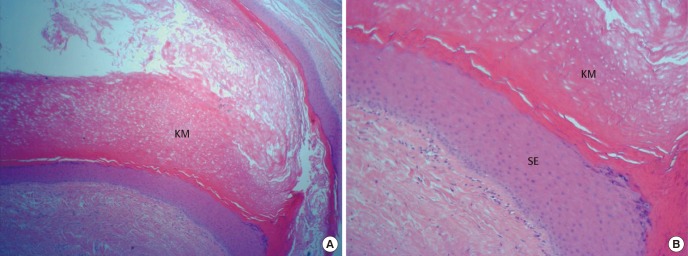
A postoperative biopsy showed keratin material (KM) surrounded by stratified squamous epithelium (SE) and a granular cell layer adjacent to the keratin-containing cyst lumen. The result was compatible with an epidermal cyst. H&E stain. (A) ×40. (B) ×100.
Epidermal cysts usually result from inflammation around pilosebaceous follicles [4]. However, no pilosebaceous follicles are present in the skin of the palm and the sole of the foot. Epidermal cysts in the palmoplantar skin have been assumed to result from the implantation of epidermal fragments due to a penetrating injury or another form of epidermal trauma [15]. Recently, some palmoplantar epidermal cysts have been reported to be caused by human papilloma virus (HPV) infection [45]. The pathophysiology of the epidermal cyst in this patient was presumed to be the implantation of an epidermal fragment, since the patient in this case had a history of recurrent occupational mechanical trauma [13]. We did not test for HPV infection because the patient did not present any symptoms or signs thereof. Epidermal cysts in the palmoplantar skin are easily confused with warts or calluses. Surgeons should be aware of the possibility of epidermal cysts in palmoplantar skin and be able to diagnose them correctly and design an appropriate treatment strategy.
Notes
No potential conflict of interest relevant to this article was reported.

