Cosmetic Lateral Canthoplasty: Preserving the Lateral Canthal Angle
Article information
Abstract
Cosmetic lateral canthoplasty, in which the size of the eye is increased by extending the palpebral fissure and decreasing the degree of the eye slant, has become a prevalent procedure for East Asians. However, it is not uncommon for there to be complications or unfavorable results after the surgery. With this in mind, the authors have designed a surgical method to reduce complications in cosmetic lateral canthoplasty by preserving the lateral canthal angle. We discuss here the anatomy required for surgery, the surgical methods, and methods for reducing complications during cosmetic lateral canthoplasty.
INTRODUCTION
Lateral canthoplasty is a procedure in which the lateral canthus is fixed (anchored) to the lateral orbital rim after surgical division (lateral cantholysis). It is usually performed with lower blepharoplasty in order to correct the laxity and malposition of the lower lid [1]. Lateral canthoplasty also can control the position of the lower lid in order to produce the desired shape of the eyelid fissure [2]. It is performed to change the eye slant [3] or lengthen the eyes [4] depending on the position of the fixation. In the West, the procedure is carried out to uplift the downward slant of the eyelid, which is usually caused by aging [3]. However, Asians do not favor this because an upward slant makes the eyes seem smaller and has a strong appearance. Therefore, cosmetic lateral canthoplasty is commonly carried out in Asia. This procedure lengthens the palpebral fissure and lowers the eye slant by moving the lateral canthus posterolaterally or posterolaterally downward. This causes the lateral scleral triangle to increase in size, making the eyes appear larger and leaving a smoother appearance.
Cosmetic lateral canthoplasty mostly includes lateral canthotomy and lateral cantholysis [4567]. However, this destroys the lateral canthal angle, and the scarring from this can lead to a variety of deformities [891011]. Therefore, the authors have designed and carried out a lateral canthoplasty which preserves the canthal angle.
In this article, we introduce a method of lateral canthoplasty which preserves the canthal angle, and discuss methods for preventing complications of cosmetic lateral canthoplasty.
SURGERY RELATED ANATOMY
Lateral canthal tendon
The lateral canthal tendon (LCT) has a superficial component and a deep component. The superficial component is a continuous extension from the orbicularis oculis muscle that is inserted into the lateral orbital rim through the thickening of the overlay whereas the deep component of the LCT diverges from the lateral end of the tarsus and adjoins Whitnall's tubercle of the lateral orbital rim [112]. However, there is controversy surrounding the naming and the anatomical relationship of the surrounding tissue [11314]. The deep portion mainly serves to provide lateral canthal support; therefore, the detachment and division of the deep portion is not recommended for ordinary cosmetic lateral canthoplasty. Instead, the superficial component should be sufficiently detached to allow the movement of the lateral canthus without tension.
METHODS
Preoperative evaluation
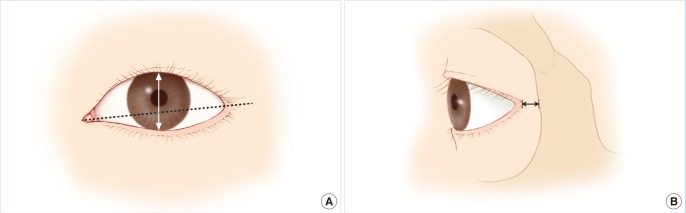
It is essential that the distance from the lateral canthus to the orbital rim and the canthal tilt be checked before surgery (Fig. 1). If the goal of the surgery is the lengthening of the palpebral fissure, the lateral canthus to orbital rim distance is important, and if the goal is change to the degree of eye slant, the canthal tilt is important. In fact, however, there are many cases in which the operation has both goals. Therefore, it is very important to conduct a preoperative evaluation of both measurements when performing cosmetic lateral canthoplasty.
Operative technique
The surgical design is as shown in the picture (Fig. 2A). The design is composed of three incision lines, a lower eyelid incision, an upper eyelid incision, as well as an incision for VY advancement. The lower incision line is drawn 2 mm below the cilia, and the upper incision line is drawn following the gray line directly below the cilia. The VY advancement incision is designed to allow the elevation of the V-shaped flap from the grey line to the palpebral conjunctiva. In some cases, the lower incision may be omitted, in which case surgical vision can be ensured by further extending the upper incision towards the lateral canthus.
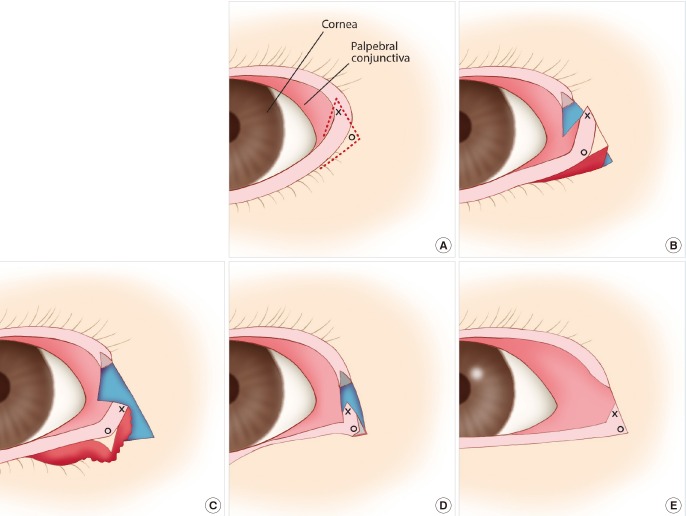
Surgical design and surgical procedure diagram
(A) Surgical design. The tip of the V-shaped flap (X) and the tip of lateral canthus (O) is indicated. (B) After the skin incision, detachment is carried out on the orbicularis oculi muscle, the superficial canthal tendon, and the pre-periosteal tissue. (C) As shown in the picture, after detachment, the lateral canthus, including the lateral canthal angle, is able to move without tension. (D) The lateral canthus is affixed at the appropriate position of the lateral orbital rim. (E) Defects of the upper eyelid are sutured by VY advancement, and surgery is concluded with the suturing of the remaining incision site.
Surgery is carried out under local anesthesia. After making a skin incision, a submuscular dissection is conducted using Tenotomy Scissors and a bipolar coagulator (Fig. 2B). After this, the exposed superficial canthal tendon is sufficiently detached. The pre-periosteal tissue should be appropriately detached, leaving a portion of tissue at the orbital rim. After this, the lateral canthus is able to move without tension as seen in the illustration (Fig. 2C). Next, the lateral canthus is fixed to the lateral orbital rim (Fig. 2D). Then, by precisely passing a needle through the tarsal plate of the lower eyelid lateral end or through the canthal tendon attached to it, and by similarly passing a needle through the periosteum and pre-periosteal tissue of the orbital rim, the sutures are tied.
After being fixed, the eyelid shape should be checked while the patient's eyes are open. At this time, the patient should be thoroughly observed for any signs of the occurrence of ptosis or contact between the eyeball and lower eyelid. Once the fixation is completed, the upper eyelid defect is sutured in a VY advancement manner, and closure of the remaining skin incision site is performed (Fig. 2E).
RESULTS
Representative cases
Case 1
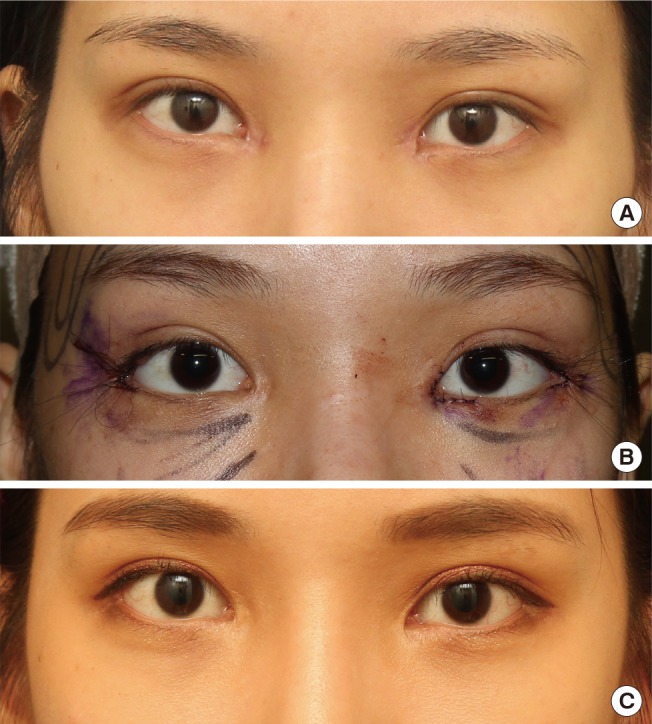
A female patient (26-year-old) presented with facial asymmetry and mild dystopia. Bilateral lateral canthoplasty was performed. The right side was overcorrected more than the left. Immediately after surgery, there was noticeable improvement of the dystopia and the palpebral fissure had been lengthened. Five months after surgery, good surgical results were still observed without any deformity of the external commissure (Fig. 3).
Case 2
A 24-year-old female patient underwent bilateral lateral canthoplasty. Photos taken one month and five months after surgery show a lengthening of the palpebral fissure and a decrease in degree of the eye slant. Deformity of the external commissure was not observed (Fig. 4).
DISCUSSION
Cosmetic lateral canthoplasty in order to lengthen the small palpebral fissure and decrease the degree of the eye slant has become prevalent among East Asians. However, as with conventional lateral canthoplasty, surgical methods that compromise the lateral canthal angle may be accompanied by complications from the procedure. Common complications include deformity of the external commissure, recurrence, mucosal exposure, and ectropion.
The first two complications may result in a reduction of the lateral white triangle, in which case patients feel as if the surgery had no effect or even that their eyes have gotten smaller [10]. Mucosal exposure and ectropion are aesthetically unpleasant and can cause eye dryness. In this paper we discuss methods to reduce such complications.
Most lateral canthoplasty methods involve conducting lateral canthotomy in order to carry out lateral cantholysis. However, the destruction of the canthal angle due to lateral canthotomy can lead to various deformities, such as webbing or rounding of the external commissure. Therefore, lateral canthoplasty methods have also been introduced which preserve the canthal angle, in order to prevent such deformities [8111516]. On the other hand, it is difficult to use lateral canthoplasty methods that preserve the canthal angle in cosmetic lateral canthoplasty. In cosmetic lateral canthoplasty, unlike conventional lateral canthoplasty, mechanical ptosis can be avoided only by separating the skin of the upper eyelid and lower eyelid because the direction of the movement of the lateral canthus is posterolateral or posterolaterally downward. In order to resolve this problem, the authors designed a method of conducting cantholysis and lateral canthotomy that preserves the lateral canthal angle, and applied this to cosmetic lateral canthoplasty. The biggest advantage of this method is that, by preserving the lateral canthal angle, there is almost no occurrence of deformity of the external commissure.
One disadvantage of this surgery is that a defect of the upper lid remains. However, as this defect is on an area covered by the cilia, if the size of the V flap is not designed to be big, it will nearly unnoticeable. In addition, if the suture layer of the V flap does not match precisely, a trapdoor scar can appear. However, as this can be fixed easily through cauterization or a simple excision, it could be considered an insignificant complication compared to a deformity like webbing or rounding. The authors are currently in the midst of collecting and analyzing patient data, and are preparing to report the results.
Recurrence, mucosal exposure, and ectropion are mainly brought about by improper fixation. The tissue that is fixed and the position of fixation are both important for the proper fixation of the lateral canthus to the orbital rim. In order to reduce the cheese-wiring effect, it is important that any fixed tissue include the tarsal plate at the lateral canthus and the periosteum at the lateral orbital rim. However, as the size of the tarsal plate near the lateral canthus becomes very small [17], it is not easy for the suture material to pass through this tissue, and depending on the circumstances, the LCT connected to the tarsal plate can be used as a fixation tissue instead. Because the thickness of the periosteum of the lateral orbital rim is comparatively thin, leaving pre-periosteal tissue when performing detachment aids in a secure fixation.
If the fixation position at the rim is too much towards the inner aspect of the lateral orbital rim, entropion of the lower eyelid can occur, whereas if the position is too much towards the lateral aspect of the lateral orbital rim, ectropion and mucosal exposure are likely to occur. In addition, if the fixation position is excessively downward, it appears unnatural and mechanical ptosis occurs. Keeping such things in mind, it is possible to prevent unfavorable results and complications stemming from improper fixation.
In conclusion, the following points should be kept in mind in order to reduce complications. Before the operation, a precise evaluation of the preoperative anatomy of the patient's eyelid should be carried out, and based on this, an appropriate surgical plan should be formulated. In addition, surgical methods should ideally preserve the maximum normal anatomy of the lateral canthus. The lateral canthus released during surgery should be securely affixed to the proper area of the orbital rim. If surgery is carried out taking these points into consideration, a suitable portion of the complications involved in cosmetic lateral canthoplasty can be prevented.
Notes
No potential conflict of interest relevant to this article was reported.