Deep-Plane Lipoabdominoplasty in East Asians
Article information
Abstract
Background
The objective of this study was to develop a new surgical technique by combining traditional abdominoplasty with liposuction. This combination of operations permits simpler and more accurate management of various abdominal deformities. In lipoabdominoplasty, the combination of techniques is of paramount concern. Herein, we introduce a new combination of liposuction and abdominoplasty using deep-plane flap sliding to maximize the benefits of both techniques.
Methods
Deep-plane lipoabdominoplasty was performed in 143 patients between January 2007 and May 2014. We applied extensive liposuction on the entire abdomen followed by a sliding flap through the deep plane after repairing the diastasis recti. The abdominal wound closure was completed with repair of Scarpa's fascia.
Results
The average amount of liposuction aspirate was 1,400 mL (700–3,100 mL), and the size of the average excised skin ellipse was 21.78×12.81 cm (from 15×10 to 25×15 cm). There were no major complications such as deep-vein thrombosis or pulmonary embolism. We encountered 22 cases of minor complications: one wound infection, one case of skin necrosis, two cases of undercorrection, nine hypertrophic scars, and nine seromas. These complications were solved by conservative management or simple revision.
Conclusions
The use of deep-plane lipoabdominoplasty can correct abdominal deformities more effectively and with fewer complications than traditional abdominoplasty.
INTRODUCTION
There has been a recent increase in the number of patients interested in correcting body contour problems. Many conditions including obesity, severe weight loss, and pregnancy cause changes in the body contour, including that of the abdominal region. The increased need for abdominal plastic surgery associated with bariatric surgery has led to the intensive development of a range of surgical techniques [1].
Liposuction and abdominoplasty have each developed their own distinct surgical concepts, techniques, and equipment. The effective combination of these two different techniques is of paramount concern in the correction of abdominal deformities, including excessive skin, excessive fat, diastasis recti, and loss of the waist line. Wide abdominal flap undermining is directly associated with flap morbidities such as necrosis, seroma, and hematoma. Other complications, such as scar hypertrophy and unexpected scar position, require special attention and surgical skill [2].
We combined liposuction of the superficial and deep fat layers of the entire abdomen, full-thickness resection of the infraumbilical ellipse, mobilization of the abdominal flap through the deep plane, and fascial repair. We named this technique deep-plane lipoabdominoplasty (DPLA).
METHODS
From January 2007 to May 2014, we performed DPLA in 143 patients to correct their abdominal contour. Four of the patients were men and 139 were women.
Ninety-seven patients suffered from abdominal changes after pregnancy, and abdominal bulging with striae gravidarum was the major postpartum problem. Twenty-four of those 97 patients had an abdominal vertical scar, 11 had a surface irregularity after liposuction surgery from other clinics, and 5 seriously obese patients (with a body mass index over 30 kg/m2) underwent surgery to treat abdominal pendulum.
Operating techniques
Design
A fusiform design was marked on the abdomen for skin excision. There are no standard practices for designing the ellipse, and the lateral point was chosen based on each patient's needs. The proposed lower abdominal incision was marked under the patient's underwear, and utilizing the pinch technique, the superior extent of the incision was approximated with minimal to no tension. It is beneficial to mark the area beneath the patient's clothing. If the patient prefers to wear low-cut jeans, it is important to hide the scar under the clothing.
Infiltration
The abdomen was infiltrated with tumescent fluid using the superwet technique. Each liter of tumescent solution consisted of 1 liter of lactated Ringer's solution, 10 mL of 1% lidocaine, and 1 mL of 1:1,000 epinephrine. The total lidocaine dose was limited to a maximum of 35 mg/mL.
External laser
After fluid infiltration, liposuction efficiency was enhanced by irradiating the abdominal surface with an EML (Erchonia Medical Co., McKinney, TX, USA) or Laserslim (Nanum Medical Inc., Seoul, Korea), for approximately 15 minutes (Fig. 1).
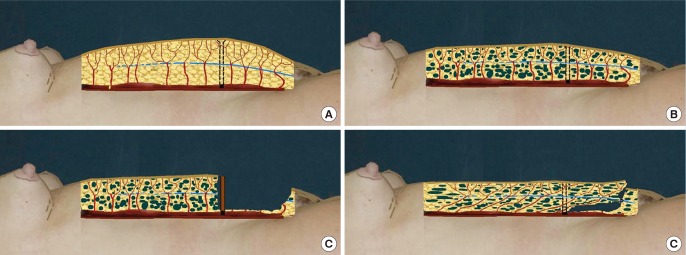
Liposuction
With the patient in the supine position, liposuction was performed over the subcostal area beneath the breast and on the infraumbilical region. A 3–4 mm cannula was used to remove the fat from the superficial and deep layers of the flank and lower abdomen (Fig. 2).
Skin excision and umbilical isolation
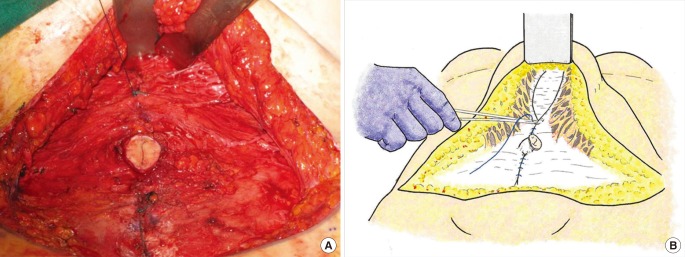
After completing the liposuction procedure, tension on the abdominal skin was relieved enough to be easily pulled down by pinching. A full-thickness resection of the infraumbilical abdominal ellipse, including Scarpa's fascia and the deep fat layer, was performed after umbilical isolation, which is consistent with traditional abdominoplasty. A small amount of deep fat was preserved over the deep fascia, especially in the bilateral inguinal regions (Fig. 3).
Rectus plication
Median abdominal undermining was performed between the medial borders of the rectus abdominis muscle. Special care was taken not to pass beyond the borders. This strategy is similar to the selective undermining of Saldanha's technique [3]. If the infraumbilical diastasis is repaired first, the width of the supraumbilical diastasis may be narrowed, making the medial border of the rectus more obvious in the upper abdomen, and thereby securing a clear visual field in the narrow tunnel (Fig. 4).
Flap sliding
If liposuction was sufficient and even, sliding of the abdominal flap was performed without difficulty. The sliding plane was below Scarpa's fascia (Fig. 5).
Wound closure
In contrast to the traditional approach, surgical closure must begin from the lateral region and move medially to ensure symmetry without creating a dog-ear deformity. The Scarpa's fascia was repaired first, and then the subcutaneous tissue and dermis were closed securely. This approach was used to reduce the tension on the midline skin closure by placing more tension laterally (Fig. 6).
Umbilical transposition
A 1.0–2.0 cm vertical elliptical excision for the abdominal flap was made in the midline overlying the buried umbilicus. A path was then created by blunt dissection for the stalk. The point of the new umbilicus was above the level of the anterior superior iliac spine or 10–15 cm over the superior border of the pubic tubercle. Three point fixation sutures at 3 o'clock, 6 o'clock, and 9 o'clock were placed on the subcutaneous layer of the abdominal flap and the umbilicus through the fascia of the surrounding abdominal wall.
Drain insertion
We used a continuous Jackson-Pratt drain for drainage over the course of three or seven days.
Skin closure
After securing the fascia and dermal suture, we applied skin bond (Histoacryl, B. Braun, Aesculap, Germany) along the incisional wounds (Fig. 7).
RESULTS
We corrected abdominal deformities without life-threatening complications, and the patients had a flat abdomen and smooth waistline after surgery (Fig. 8).

Case
A 42-year-old woman with bulging and striae gravidarum underwent deep-plane lipoabdominoplasty. (A) Before surgery. (B) After surgery.
The average follow-up period was 12.1 months (range, 2–40 months). Seventy-three patients had undergone natural childbirth, fifteen patients had undergone one Caesarian section, and nine patients had experienced two Caesarian sections. The average height of the patients was 161.12±4.65 cm and their average body weight was 55.59±7.56 kg. On the basis of the 2000 World Health Organization Western Pacific Regional Office criteria [4], most patients had a body mass index within the normal range (mean, 21.50±2.95 kg/m2). The average weight of the resected abdominal tissues was 194.88±139.99 g, and the average dimensions of the excised skin were 21.78±6.77 cm× 12.81±4.16 cm, with an area of 279.00±136.93 cm2. The average infiltration volume of the tumescent solution was 1,646.91 ±699.41 mL, and the volume of liposuction was 1,384.86± 884.78 mL.
Twenty-two patients experienced complications. One patient (0.88%) suffered from a localized wound infection that was resolved by conservative treatment. Skin necrosis was observed in one patient (0.88%), who required serial debridement and vacuum-assisted closure. Additional liposuction was performed in two undercorrected patients (1.77%). Nine patients (7.96%) with hypertrophic scars underwent scar revision. Seromas occurred in nine patients (7.96%). Serial needle aspiration and compressive dressing were performed in two of the nine patients. In the other seven patients, fibrin glue (Tisseel-Fibrin Sealant, Baxter AG, Vienna, Austria) was used for hemostasis, and a Jackson-Pratt drain was reapplied. The complications were successfully treated within seven days. No severe complications, such as deep-vein thrombosis or pulmonary embolism, occurred.
DISCUSSION
History of the extent of undermining and the use of Scarpa's fascia
Abdominoplasty consists of pannus excision, muscular tightening, and skin redraping for an hourglass waistline. The history of abdominoplasty began in the late 1960s.
Vernon successfully standardized the use of extensive undermining to allow easy flap mobilization and umbilical transposition [5]. After Illouz [6] developed the liposuction technique, the evolution of abdominoplasty accelerated. In 1985, Hakme [7] introduced the mini-abdominoplasty with liposuction, and beginning in 1991, Matarasso [8] recommended safe areas of abdominal circulation and dissection in his articles. In 1992, Illouz [6], Avelar [9], and Shestak [10] suggested advanced techniques of minimal to zero undermining accompanied by liposuction. In 1995, Lockwood [11] reported the high lateral tension abdominoplasty (HLTA) using Scarpa's fascial closure to decrease the tension of the abdominal flap. According to Rosenfield's [12] revision of the HLTA, Scarpa's fascial closure makes it possible to retract the skin more effectively and to remove the excess skin aggressively, especially in the central abdomen. Saldanha first reported the use of lipoabdominoplasty combined with aggressive liposuction and mobilization of the superficial abdominal tissue in 2002.
Concept of the DPLA technique
Extensive and aggressive liposuction without undermining
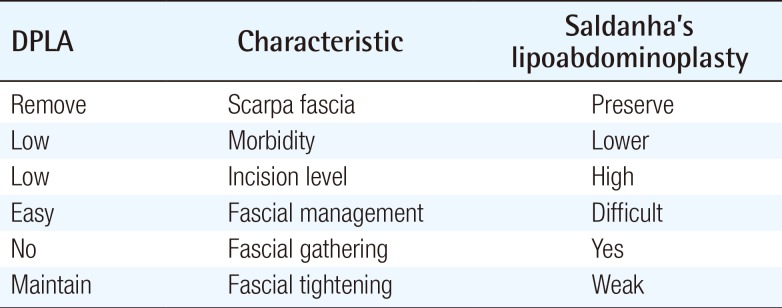
Traditional abdominoplasty has an area of limited dissection or liposuction in order to avoid the deterioration of flap circulation, as Matarasso [8] argued. Abdominal undermining makes it difficult to reduce the thickness or excessive skin in the upper abdomen. Many surgeons currently perform a limited midline dissection during abdominoplasty. However, the area of limited dissection includes many central perforators from the deep epigastric vessels, especially in the periumbilical area (Fig. 9). It is critical to avoid dissecting the anterior surface of the rectus abdominis muscle as much as possible. Instead of undermining, we applied extensive and aggressive liposuction over the entire abdominal portion of the rectus muscle. Dissection was performed only over the area of diastasis recti. This made it possible to save the majority of the abdominal perforators and to mobilize the abdominal flap through the deep plane. Additionally, it led to an absence of dead space for seroma formation in the epigastrium.
Preservation of the abdominal perforators
(A) We were able to preserve many central perforators (the area marked in green) by dissecting the anterior surface of the rectus abdominis muscle to the minimal extent possible. (B) Intraoperative photographs of the limited dissection of the abdominal flap.
Through the liposuction of superficial and deep fat, abdominal thickness can be managed while maintaining the abdominal perforators, especially from the deep epigastric vessels. This makes the abdomen a multi-pedicled neurovascular flap. After removal of superficial and deep fat, a sufficient sliding space is prepared, which is called 'mesh undermining.'
In fact, in the epigastric area, Scarpa's fascia is not definite. Monoplane premuscular liposuction is therefore likely to be performed in this area. In the umbilical area, however, it is possible to distinguish between the deep and superficial planes by the clear presence of Scarpa's fascia [13].
Plication of the rectus fascia
Rectus diastasis was repaired during surgery, and the medial borders of the rectus sheath were approximated without incising the sheath (Fig. 4). A continuous suture was placed midway between the xiphoid and pubis. It is important not to overlap to secure the plication, because the rate of recurrence of diastasis is higher in overcorrected cases [14].
Resection of the abdominal ellipse and sliding of the abdominal flap
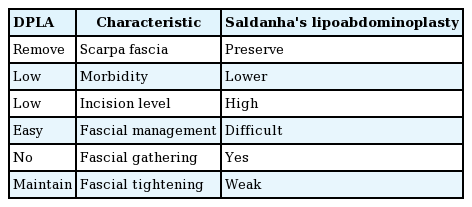
Recently, Saldanha's lipoabdominoplasty has shown outstanding achievements in abdominal plastic surgery. On first glance, DPLA appears similar to Saldanha's technique, but significant differences are present between these two techniques with regard to tissue removal and mobilization of the abdominal flap.
Saldanha stated that the superficial liposuction technique introduced by De Souza Pinto is one of the fundamental pillars of lipoabdominoplasty, because it provides more mobility to the abdominal flap so that it can slide down easily and reach the suprapubic region. In his technique, the infraumbilical superficial tissue is removed, and the superficial tissue of the upper abdomen beyond Scarpa's fascia is lowered [1215].
In DPLA, the removal of the lower abdominal tissue from the skin to the deep fat layer, including Scarpa's fascia, takes place in an en bloc pattern, which makes it possible to mobilize the flap above the deep fascia and to manipulate Scarpa's fascia.
When the lower abdominal excess is removed, it is important for a certain amount of deep fat attached to the deep fascia to be preserved, especially in the bilateral femoral regions (* in Fig. 3). This preserves important lymphatic channels to help drain the lower abdomen region and reduce seroma and edema formation [1617].
Moreover, it is easier to plicate diastasis recti through the defect after the excision of deep tissue than when Scarpa's fascia and deep fat remain present. The rectus plication procedure can be helpful in producing an hourglass-shaped waistline.
As a result of liposuction, the deep fat layer acts as the deep plane, between the rectus fascia and the Scarpa's fascia, and as the sliding surface (Fig. 5). The skin can be easily approximated so that it is not necessary to flex the hip. The repair of Scarpa's fascia plays an important role in this procedure for multiple reasons. Through fascial closure, the tension is relieved and the disturbance of dermal circulation is solved. Moreover, it allows high lateral tension abdominoplasty to be performed, since skin tension is created in the lateral region, rather than in the central region, as in traditional abdominoplasty. This aspect of the HLTA technique is helpful for securing the circulation of the low-central skin of the flap and for removing a sufficient amount of upper abdominal skin [12].
Repairing Scarpa's fascia can lead to the scar developing in a lower position [12]. Patients currently often show a preference for low-cut clothing, and the scar must therefore be hidden under the clothes, which requires a lower incision. During preoperative marking, it can be helpful for the patient to wear underwear or his or her preferred clothing. After wound closure, the lower abdominal skin is slightly pulled upward, which moves the scar to a higher location. This may be more severe when Scarpa's fascia is not repaired, because the skin is the only tension-bearing structure. Suspending Scarpa's fascia limits scar migration. Additionally, the resulting lower tension of the central region of the flap prevents superior displacement of the pubic area. The upward migration of the pubic hair and the mons pubis has an unfavorable aesthetic effect, especially in East Asians, who tend to have broader pubic regions than Caucasians.
In 2008, Rangaswamy [18] reported on a new lipoabdominoplasty technique that was similar to DPLA. However, DPLA is different from Mohan's technique in several ways. First, liposuction was performed on both the superficial and deep layers of the fat. Liposuction from the superficial to the deep plane further increases the mobility of the flap and reduces abdominal fat volume relative to liposuction only on the deep plane. Second, flap elevation was performed with the minimal width, which was limited to between the medial border of the rectus abdominis muscle in order to spare the abdominal perforator. Third, plication was carried out from the inferior to the superior side. This cleared the visual field for delicate manipulation. Finally, we resected the full layer of the lower abdominal tissue including Scarpa's fascia and the deep fat layer. This reduced the fullness around the closed abdominal wound more than Mohan's technique [13].
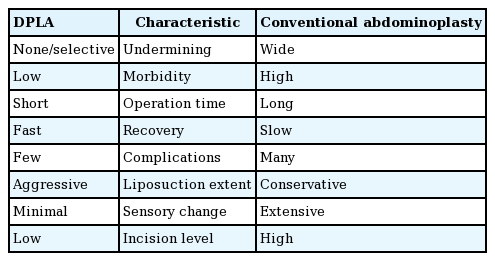
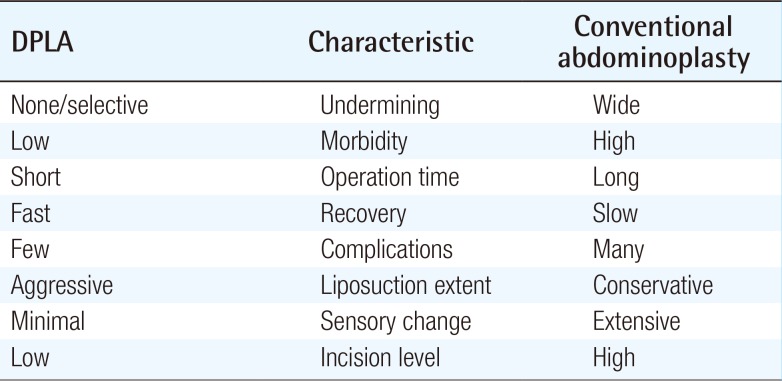
Compared with traditional abdominoplasty, DPLA has many advantages, such as a shorter surgical time and recovery time, less flap morbidity, and less sensory disturbance with fewer complications (Table 1). In comparison with Saldanha's lipoabdominoplasty, DPLA has several advantages, such as a lower incision level, easier musculofascial manipulation, the absence of fascial overlapping, and a long-term fascial tightening effect (Table 2). Using DPLA, we were able to correct abdominal deformities more effectively with fewer complications in comparison with traditional abdominoplasty.
Notes
No potential conflict of interest relevant to this article was reported.