Sublabial Autologous Ear Cartilage Grafting for Increasing the Nasolabial Angle
Article information
Abstract
Background
The loss of nasal tip support is caused by many factors and eventually results in the collapse and eventual dropping of the nasal tip. This reduces the nasolabial (NL) angle and negatively affects respiratory functions and one's appearance.
Methods
The aim of this retrospective study, which was conducted on 52 patients, was to present and popularize a simple and effective method for the reconstruction of a weakened columella by inserting an autologous ear cartilage graft using a sublabial approach.
Results
Of all the patients, three patients experienced transplant rejection. The period of follow-up observation was one to five years (mean, 27 months). The results were objectively evaluated by measuring the NL angle in standardized photos before and after the procedure at different time intervals over the follow-up period. We observed a significant increase of the NL angle (mean, 20°), and found these results to be durable over the long term. Of the 52 patients included in this study observed patients, three were dissatisfied (due to immediate infection and shifting of the strut), 28 were satisfied, and 21 were very satisfied.
Conclusions
The surgical method described here is simple and can be learned quickly. It has very good results with few complications, and is our method of choice for complex and serious cases seen in everyday rhinosurgical practice.
INTRODUCTION
A major problem in cosmetic surgery, if not the largest problem, is the collapse of the tip of the nose, which manifests as reduction of the nasolabial (NL) angle and the loss of nasal tip projection. This process occurs due to the loss of mechanical and structural support of the nasal tip, which can be caused by factors including unfavourable anatomical characteristics of the alar and upper lateral cartilage, the septal cartilage, and its ligaments [1]; ethnically specific anatomical features [234]; the aging process [56]; the influence of gravity; the size of the nose; previous nose or septum surgery [7]; the loss of the upper incisors and upper alveolar ridge atrophy; and trauma and infections of the nose and its supporting structures. Correction of this deformity requires relatively complex operating procedures [891011].
The columellar strut [121314] is one of the most important solutions to this difficult problem in both functional and aesthetic rhinoplasty. The most logical solution to the problem of a distorted nose tip lies in solid tissue implantation, which, in this case, is made out of the patient's own cartilage.
There are not many ways to place the strut in the columella [1215]. Today, the strut is usually placed using the open rhinoplasty method [14], but this technique does not adequately address how to perform operations in which only the nose tip needs to be raised, while simultaneously preserving the integrity of the nose. Therefore, we developed a method that is superior to previous methods in terms of the ease of strut placement.
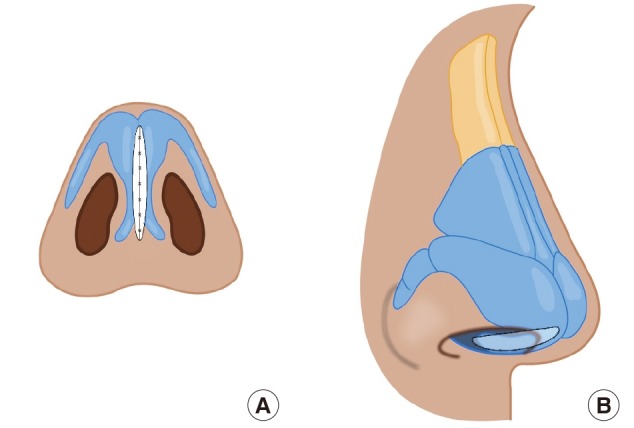
Our method involves a sublabial approach to the anterior nasal spine, in which a pocket is made between the medial crura of the alar cartilages, in front of the caudal edge of the septum [121617]. This pocket is used to insert the cartilage.
Every surgical procedure was preceded by a detailed nasal examination and analysis of the relationship of the soft tissues of the face and nose, with a focus on the profile [18]; an assessment of whether surgery was previously performed on the nose; visualization of the NL angle; rhinoscopic examination; and palpation and use of pressure on the nose tip, which provides insight regarding the degree of nose tip collapse.
METHODS
Other methods
Many other methods have been developed for raising the nasal tip. To a greater or lesser extent, the following techniques are standard procedures in the rhinosurgical armamentarium: the umbrella or T-graft developed by Peck and Heiden [19], medialization of the medial crura of the alar cartilage, the premaxillary graft, the shield-tip graft developed by Sheen and Sheen [20], the lateral crural steal technique [81014], medial crural-caudal septal imbrication, the tongue-in-groove technique [101721], the contoured auricular projection graft developed by Porter et al. [22] as an alternative to the onlay graft developed by Sheen, and various other types of nasal tip grafts [71423].
Surgical techniques
Over the past 15 years, we have developed a surgical method for raising the nasal tip in cases where the NL angle is significantly lower (by more than 10°) than to the standard 90°, and where the nasal tip shows drooping.
Preparation and insertion of cartilage
We use the retroauricular approach to remove a relatively large piece of cartilage (approximately 1.5 cm×3 cm) from the cavum conchae area and fold it in the middle by applying an incomplete longitudinal cut. The free edges of the graft are stitched with nonabsorbable 6-0 sutures. In this manner, we obtain a solid, massive graft that will resist resorptive changes and at the same time be statically superior.
If a strut made this way is bent to one side, it is corrected with appropriate 6-0 nonabsorbable mattress sutures (e.g., Ethilon).
The dimensions of the strut are 2.5–3.0 cm in length and 0.5–0.7 cm in width (Figs. 1, 2).
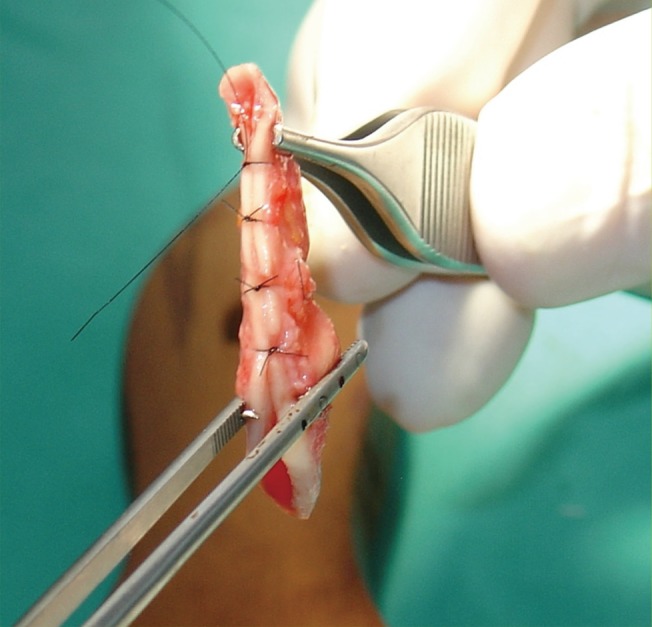
A folded strut in situ
Intraoperative view of a folded strut with mattress sutures ready for insertion.
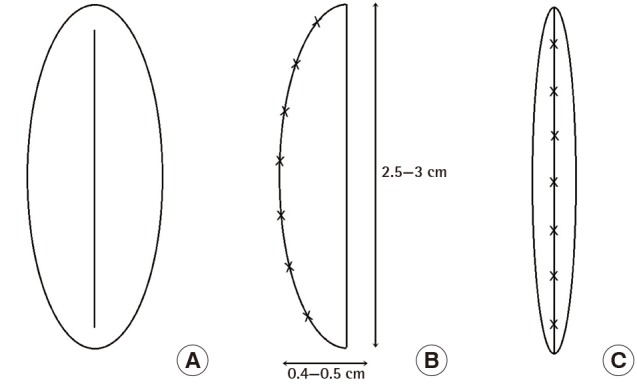
Preparation of a folded strut
A sketch of the cartilage graft used in this technique. (A) Cartilage graft with a longitudinal incision. (B) Side view of the folded strut ready for insertion. (C) Frontal view of the folded strut with mattress sutures ready for insertion.
Before the implant is inserted, a pocket is formed using a sublabial approach and a small 1-cm horizontal incision is made in the gingival sulcus of the frenulum. Further access to the anterior nasal spine is made with scissors, and a pocket is made behind and between the medial crura of the alar cartilages. The pocket should not be too wide, it should not extend too far towards the caudal part of the septum, and it must not extend under the skin of the nasal tip (Fig. 3).
Placement and insertion of the implant
The columella is held with the thumb and forefinger of the left hand while the implant is taken with Adson-Braun forceps and, as gently as possible, inserted into the pocket, making sure that it does not extend under the skin of the tip (Fig. 4). When the implant is placed, the distal part of the implant is located directly in front of the anterior nasal spine on the premaxilla, and it is then fixed with absorbable sutures (e.g., Vicryl 4-0). During the fixation of the implant, it is necessary to verify that the implant is well centred and positioned in the middle of the columella. Sometimes, if under relatively strong tension, it must be shortened. Before closing the incisional wound, the pocket is rinsed with an antibiotic (gentamicin).

Intraoperative strut insertion
Insertion of the folded strut into the pocket using Adson-Braun forceps and scissors, ensuring that it does not extend under the skin of the tip. (A) The scissors hold the pocket open and lead the strut into the correct position. (B) Final adjustment of the strut into the desired position using Adson-Braun forceps.
Insertion of the cartilage implant is a highly effective and simple surgical method. The procedure takes 40 minutes, is performed under local anaesthetics with sedation, and has a low rate of complications and failure.
It can be performed independently as a single surgical procedure for raising the nasal tip or as part of a complete rhinoplasty. It is equally effective in both primary and secondary rhinoplasty.
Primary rhinoplasty involves treating a retracted columella, a hanging and drooping nasal tip, and reduced projection of the nasal tip. In secondary rhinoplasty, this method is used on a retracted columella, a collapsed nasal tip caused by the over-resection of supporting structures, or after septoplasty in which the nasal tip has dropped due to distal over-resection and the resection of other parts of the cartilaginous septum. This method can also be successfully applied in cases of septal perforation stemming from various causes and resulting in drooping of the nasal tip.
The surgical technique described above allows stabilization of the nasal tip, which becomes firm to the touch and no longer droops. The volume and projection of the columella are increased, while the NL angle is significantly increased to the point of no longer being acute. The specific outcomes vary from case to case (Figs. 5, 6, 7).

Increased nasolabial angle in a male patient
Increase of the nasolabial angle and nasal tip projection via strut insertion after severe collapse of the nasal tip due to an athletic injury (boxing) in a male patient. (A) Preoperative nasolabial angle, 79°. (B) Postoperative nasolabial angle, 108°.

Increased nasolabial angle in a female patient
A female patient with a large nose and a collapsed nasal tip due to the lack of septal cartilage support. The nasolabial angle was measured before and after strut insertion and rhinoplasty using a closed approach. (A) Preoperative nasolabial angle, 108°. (B) Postoperative nasolabial angle, 120°.

A patient before and after cartilage strut insertion
A male patient with a large nose and a collapsed nasal tip due to the lack of septal cartilage support. The nasolabial angle was measured before and after strut insertion and rhinoplasty using a closed approach. (A) Preoperative nasolabial angle, 64°. (B) Postoperative nasolabial angle, 93°.
Definition of the nasolabial angle
The NL angle is the angle between the lower edge of the columella (the line that connects the lower edge of the columella to the subnasal point) and the upper lip (a line tangent to the upper lip and subnasal point). This angle is ideally 100°–105° in women and 95°–100° in men [2425].
Patients and methods
In this retrospective study, we analysed the photographs of 52 patients treated in our private practice from 2006 to 2010. Follow-up observations were made over one to five years, and standardized photographs were taken before and after the placement of a NL strut.
We measured the increase in the NL angle after surgery. Of the patients included in this study, 33 were female and 19 were male. The mean age of the women was 37 years, while the average age of the men was 38 years. The follow-up period ranged from one to five years (mean, 27 months).
Informed consent was obtained from all patients, as well as authorization for photographs, according to the guidelines of the American Society of Plastic Surgeons.
RESULTS
Statistical analysis was performed using Microsoft Office Excel 2007, Microsoft Corporation, Redmond, WA, USA; Minitab, Minitab Inc., State College, PA, USA; SPSS ver. 21.0., IBM Co., Armonk, NY, USA.
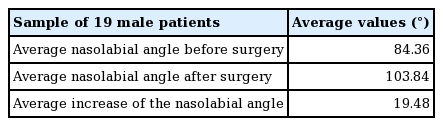
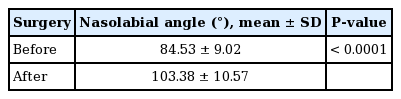
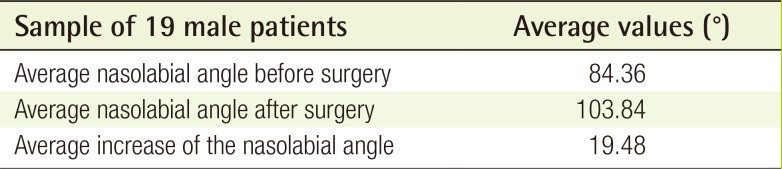
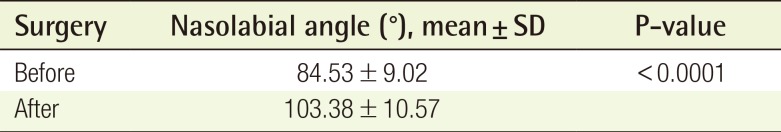
Data before surgery
The average value of the NL angle in the 19 male patients before surgery was 84.36° (Table 1), compared to 84.64° in the 33 female patients (Table 2). No statistical analysis was performed to compare these figures, because they were essentially equivalent clinically.
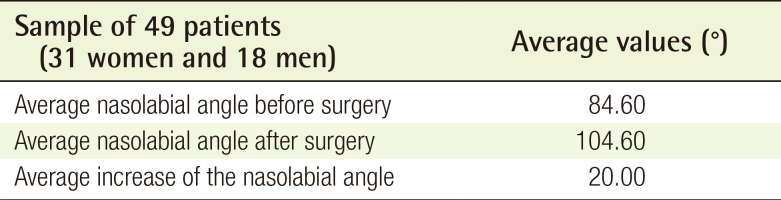
Data after surgery
The average values of the NL angle in the male patients after surgical intervention was 103.84° (Table 1), compared to 103.12° in the female patients (Table 2). The average increase of the NL angle after surgery was 19.48° for the male patients (Table 1) and 18.48° for the female patients (Table 2).
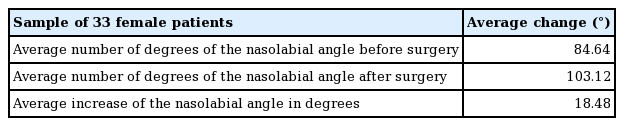
If the three patients who experienced postsurgical complications in the form of infections and graft displacement are excluded, we attained an 20° increase of the NL angle on average in the entire study population of 49 patients (31 women and 18 men) (Table 3).
Statistical analysis of the all patients showed a significant increase in the NL angle (P<0.0001) (Table 4).
In follow-up examinations conducted in the first 26 months after surgery, the average increase of the NL angle was 19.72°, while in follow-up examinations conducted more than 26 months after the operation, the average increase of the NL angle was 18.03°. These results clearly indicate that our augmentation of the NL angle was stable over time.
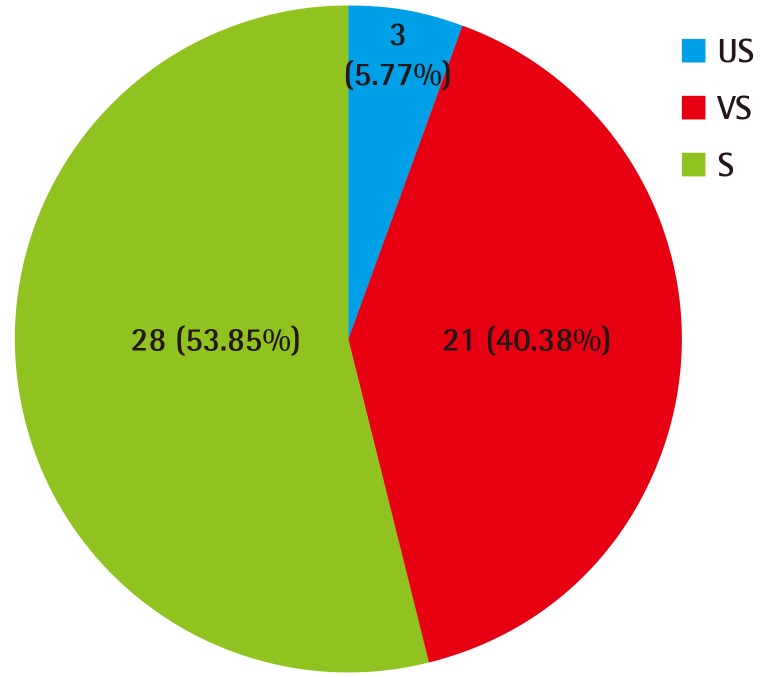
Patient satisfaction
In cosmetic surgery, patient satisfaction with the outcomes of a procedure is a very important factor. Although satisfaction is subjective and based on an individual's evaluation of a surgical result, we objectively evaluated outcomes by measuring and comparing the NL angle before and after the surgical procedure.
In cosmetic surgery, a range of methods are used to evaluate patient satisfaction. In this study, we used a simple three-option scale to evaluate patient satisfaction after aesthetic nose correction. Of the 52 patients, three were dissatisfied (due to immediate infection and shifting of the strut), 28 were pleased, and 21 were very pleased with the results (Fig. 8).
DISCUSSION
Due to the complex and variable anatomical and anthropometrical relations in the area of the upper lip, premaxilla, anterior nasal spine, columella, and nasal base [18], establishing exact criteria for defining a droopy nasal tip is exceptionally difficult. Therefore, for this research, we focused solely on measuring changes in NL angles before and after surgical procedures in which our novel method was applied.
The use of an autologous cartilaginous double-folded implant as a strut has proven to be ideal for the aforementioned indications. Septal cartilage is too thin, inadequate, or not solid enough for achieving the above results.
We used a sublabial approach in these patients because, after years of experience, we have found that graft insertion through a transfixion incision leads to a higher incidence of infection and transplant rejection. Using sublabial access, we experienced only two cases of infection and one case of graft shifting. These patients underwent surgery at the beginning of the observed series, and as our techniques improved (flushing of the implantation pocket with antibiotics, faster implantation, and precise closing of the incision), we no longer had any cases with major complications.
Moreover, we realized that the transplant must be placed into the pocket without physical contact with the nasal cavity, because the nasal cavity is always contaminated. This led us to perform this surgery as a separate surgical procedure in most cases.
Notes
No potential conflict of interest relevant to this article was reported.