Full Thickness Burn on the Finger due to Pulse Oximetry during Magnetic Resonance Imaging in a Conscious Patient
Article information
Magnetic resonance imaging (MRI) is a safe and accurate radiologic tool [1]. However, there is also a risk of physical injury or thermal injury [12]. During MRI scanning, wearing monitoring equipment containing metal such as pulse oximetry and ECG monitoring leads can cause contact burns; a few cases of thermal injury during MRI scanning in unconscious patients have been reported [12]. However, no case has been reported in conscious and sensible patients during these situations.
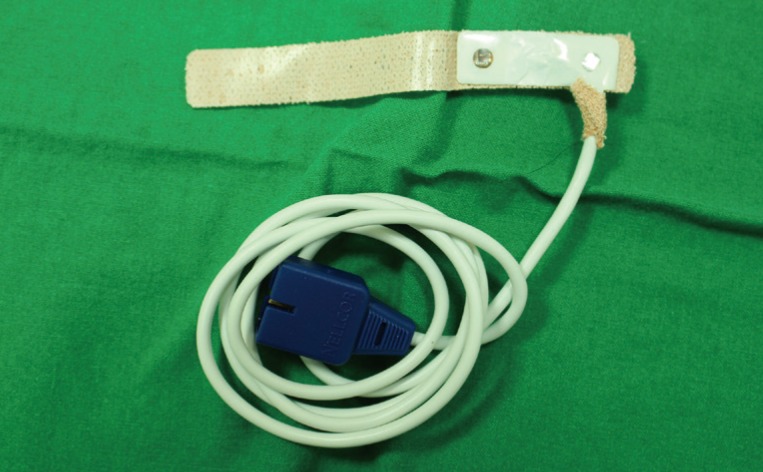
In May 2015, a 57-year-old male patient came to the emergency department of our hospital for multiple trauma. While undergoing MRI examination for a cervical spine fracture with pulse oximetry (Fig. 1) on his left index finger, he suffered a third-degree contact burn on that finger (Fig. 2). After 2 weeks of dressing, a homodigital island flap operation was performed, and 2 months after the operation, the wound had completely healed and the finger had full range of motion (Fig. 3).

Third-degree contact burn. A third-degree contact burn occurred on the distal phalanx of the left index finger. Eschar formed on the site of the injury.

Two months after the operation. At two-month follow-up, the surgical site had completely healed, with no limitation of motion.
In most cases of thermal burn induced by pulse oximetry during MRI, the patient has been sedated or in a nonverbal state [12]. Even to alerted patients with normal senses, such burns are caused by staff negligence. The most common is that patients still have the pulse oximetry that should be removed before MRI. The antenna effect between MRI and pulse oximetry comes into effect so instantly that full-thickness burn is already caused before patients recognizes and removes the pulse oximetry [3]. Extreme caution is required for removal of pulse oximetry before MRI examination.
Notes
No potential conflict of interest relevant to this article was reported.