Primary Necrotizing Fasciitis of the Breast in an Untreated Patient with Diabetes
Article information
Necrotizing fasciitis (NF) is a soft tissue infection that can be fatal. Diagnosis may be delayed because NF is easily misdiagnosed as an abscess or cellulitis [1]. It is commonly found in the extremities, perineum, and abdominal wall, but rarely in the breast. NF of the breast can be caused by previous surgery (e.g., mastectomy, implant augmentation) or trauma [2]. In this report, we present a rare case of primary NF of the breast in a patient with untreated diabetes.
A 31-year-old female patient presented to the emergency department with a 5-day history of skin color change, pain, and swelling in the left breast. The patient had been diagnosed with diabetes 6 years before, and had discontinued insulin treatment for the last 2 years. The patient reported no trauma and nor any previous surgical procedure on the breast, which was markedly swollen and erythematous. A patchy, purple and black eschar was observed in the medial area of the left breast (Fig. 1). Chest enhanced computed tomography revealed a fluid pocket approximately 9 cm in diameter with an air bubble in the left breast (Fig. 2). An emergency operation was performed to debride the necrotic skin and soft tissue. The disease was diagnosed as NF. After several debridements, the defected area was covered by a latissimus dorsi musculocutaneous flap and a full-thickness skin graft (Fig. 3). There were no complications, and the patient was discharged after two weeks.

Initial photograph in the emergency department. A 31-year-old female patient presented to the emergency department with left breast skin color change, pain, swelling, and discharge.

Initial chest ECT of the patient. There was an approximately 9-cm fluid pocket with an air bubble in the left breast, with edematous swelling and overlying skin thickening. ECT, enhanced computed tomography.
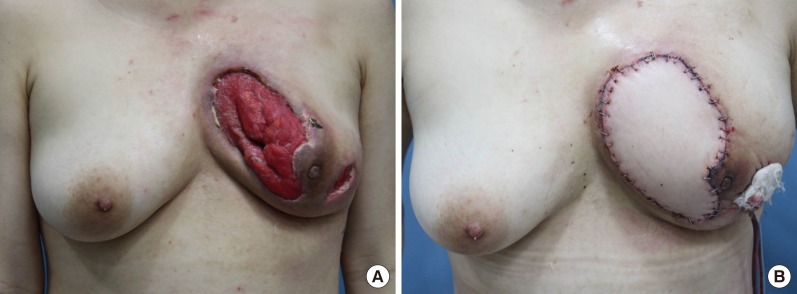
Preoperative and postoperative photos of the patient. (A) After several debridements, extended defects remained through the skin and soft tissue in the left breast. (B) The defects were covered with a latissimus dorsi musculocutaneous flap and a full-thickness skin graft.
We experienced and report here a case in a young female patient of primary NF of the left breast that was successfully treated and reconstructed. To our knowledge, this is a rare case of a patient without previous trauma that spontaneously developed NF.
Notes
This article was presented as a poster at the 6th Research and Reconstructive Forum on April 4–8, 2016 in Daegu, Korea.
No potential conflict of interest relevant to this article was reported.