Emergency Transplantation of Free Flap between Separated Thoraco-Omphalopagus Conjoined Twins
Article information
Conjoined twinning is one of the most uncommon congenital anomalies. Spencer has reported that while the incidence of conjoined twinning is close to one in 200,000 live births, 1% of all conjoined twins are stillborn and 40%–60% die shortly after birth [1]. The separation of conjoined twins presents a unique challenge to many pediatric surgical specialties. A multidisciplinary approach is essential for successful twin separation. A variety of methods for providing soft-tissue coverage have been reported in the literature and include the use of skin grafts, skin substitute products, local skin flaps, and tissue expansion.
Here, we report a case of the transplantation of a latissimus dorsi musculocutaneous (LDMC) flap between separated thoraco-omphalopagus conjoined twins.
A set of male thoraco-omphalopagus conjoined twins were born with joined manubrium and upper abdomen (Fig. 1). They had a fused liver, and each had a congenital heart anomaly. Computed tomography (CT) revealed that conjoined twin 1 had supracardiac total anomalous pulmonary venous return, dextrotransposition of the great arteries, and a perimembranous ventricular septal defect, while conjoined twin 2 had supracardiac total anomalous pulmonary venous return.
Although the literature recommends that separation should be delayed until the twins gain weight, the unstable hemodynamics and deteriorating conditions of the infants prompted early surgical separation on the 14th day after birth. During the separation, an atrial connection was identified and conjoined twin 2 took most of the fused atrium. After separation of the fused heart and liver, a chest and abdominal wall defect resulted, which was larger than expected. Closure of the defect was not performed immediately because the cardiac status of the babies required further correctional surgery.
The next morning, however, the heart of conjoined twin 1 ceased to beat and resuscitation for 5 hours failed. Then, to utilize the tissue of conjoined twin 1 for coverage of conjoined twin 2, emergency tissue transplantation was elected. An LDMC flap was chosen because of its widest dimension. An extended LDMC flap 11 cm×8 cm was designed on the donor baby's right side back, incorporating the skin from the scapula to the pelvis. After skeletonization of the thoracodorsal artery and concomitant veins, the flap was harvested from conjoined twin 1 (Fig. 2). The right third rib cartilage of conjoined twin 2 was partially removed to expose the internal mammary artery and vein. Anastomosis of the vessel was achieved with 10-0 nylon sutures. The estimated ischemic time was longer than 8 hours. After applying acellular dermal matrix over the pericardium and intestine, we attempted to cover the whole defect with the flap, but an abrupt drop of the blood pressure by the cardiac tamponade effect followed. Then, we decided to leave part of the defect open and fixed the flap along the right margin of the defect (Fig. 3). The flap showed serious congestion immediately after the anastomosis but improved gradually.

Tissue transplantation was decided, and the latissimus dorsi musculocutaneous flap was chosen to cover the thoraco-abdominal defect. The latissimus dorsi musculocutaneous flap measuring 11 cm×8 cm was designed on the back of 15-day-old conjoined twin 1. The flap was harvested with thoracodorsal artery and vein with a length of about 2.5 cm.
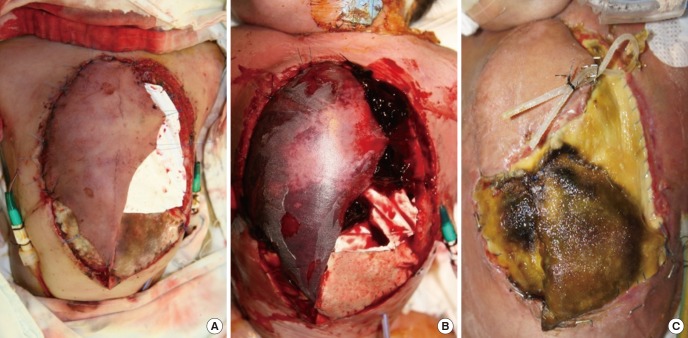
The thoracoabdominal wall could not be totally covered with the latissimus dorsi myocutaneous free flap; therefore, Permacol was applied to the remaining defect measuring about 12 cm×7 cm. (A) Immediately after flap transfer, generalized congestion was noted. (B) On postoperative day 2, the peripheral of the flap started to necrotize. (C) After debridement of the devitalized part, two-thirds of the flap survived and functioned as the covering of the heart on postoperative day 42.
After 3 weeks, two-thirds of the flap was found to survive after debridement of the necrotized margin and functioned as a covering of the heart. The rest of the defect was planned to be closed later, but the baby could not recuperate and failed to survive until day 100. The cause of death was the eventual failure to maintain the cardiac output.
The role of plastic surgeons in the separation of conjoined twins is to provide sufficient soft tissue coverage to the body wall. Skin grafting from one twin who had died to the other twin was reported by Lehr et al. [2]. Currently, various skin substitute products are available and can be used to cover deficient areas of the skin and even to reconstruct fascial defects. Random pattern or arterialized flaps of skin or skin and muscle can be used for coverage. Jackson et al. [3] reported the use of bipedicled rotational flaps of the expanded skin and local tissue adjacent to the defect when the expanded soft tissue alone proved to be insufficient for closure by simple advancement. After the first report of the successful use of tissue expansion by Zuker et al. [4] in 1986 for the separation of an ischiopagus conjoined twin, numerous reports have followed using tissue expansion in both the intraperitoneal and subcutaneous positions.
To the best of our knowledge, our case is the first case of free flap transfer for a soft tissue defect from one twin to the other twin after the separation of conjoined twins. A case of free flap transfer in neonates was reported by Van Landuyt et al. [5]. They used a thoracodorsal artery perforator free flap successfully for the skin necrosis of an 11-week-old premature boy who weighed 1,160 g. We performed free flap transfer for the 15-day-old baby who weighed 2,410 g.
Unfortunately, however, the defect after the separation of the thoraco-omphalopagus type of conjoined twin could not be successfully covered with a unilateral LDMC free flap. The defect could have been closed if we had used bilateral LDMC free flaps. There were two limitations in our case. First, elevation of the LDMC flap was done after failed resuscitation of the donor baby. During the elevation of the flap, the heart of the donor baby ceased to beat and there was no blood flow onto the LDMC flap. The other limitation was that flap elevation and recipient preparation were not performed simultaneously due to the unavailability of the operating room and equipment. Therefore, the ischemic time of the LDMC flap was more than 8 hours, which might be one of the reasons for the initial flap instability and partial flap loss.
We were able to successfully transplant a musculocutaneous flap with microvascular anastomosis in the 15 day-old newborn baby weighing 2,410 g. This case also revealed the graveness of the defect after separation of the thoraco-omphalopagus conjoined twins and the importance of addressing and discussing calculative planning for the utilization of the available soft tissue, as well as that of vital organs such as the heart and the liver, before the separation of conjoined twins.
Notes
No potential conflict of interest relevant to this article was reported.
