Acellular Dermal Matrices and Paraffinoma: A Modern Tool for a Nearly Obsolete Disease
Article information
Abstract
Paraffinoma is a destructive complication of paraffin oil injection, usually associated with massive tissue destruction, thus requiring radical surgery and subsequent complex reconstruction. Although breast and penile paraffinomas have been widely described and their management is quite standardized, paraffinomas of the knee are still rare and only few case reports or small case series are available in the current literature. We describe the case of a 77-year-old man with a large paraffinoma of the right knee that occurred after self-injection of paraffin oil, 58 years before. He underwent wide surgical resection of the soft tissues overlying the knee and subsequent two-stage reconstruction by using acellular dermal matrix and, after 20 days, split-thickness skin grafts. Follow-up after 16 months showed no signs of skin ulcerations or inflammation, with an overall improvement in function. Even though conventional flap reconstructions may be still useful, the authors believe that acellular dermal matrices represent a safe, reliable, and less invasive alternative for challenging soft tissue reconstructions even in elderly patients with multiple medical problems.
INTRODUCTION
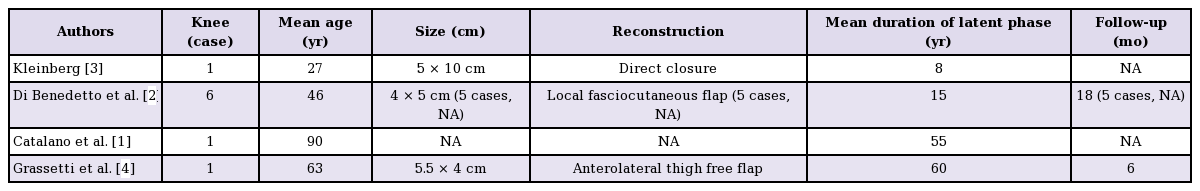
Paraffin oil injection is an old and obsolete procedure that has been used all over the world both for therapeutic and aesthetic purposes. It was introduced into medical practice around 1900 as a filler for subcutaneous defects; since then, it was largely adopted as a useful tool for the management of rhinological deformities, palatal defects, hernia repairs, pulmonary tuberculosis (as an alternative to surgical thoracoplasty), treatment of baldness, breast, penile, and facial augmentation. Furthermore, some cases of self-injection into the upper and lower limbs to avoid compulsory military service have been reported. Unfortunately, despite the initial good results, several short- and long-term destructive complications were described due to the migration and deposition of paraffin, and this procedure was therefore abandoned [12]. After the immediate inflammatory reaction, patients usually reported a relatively long latent phase, finally resulting in the formation of multiple foreign body granulomas known as paraffinomas, which are associated with massive tissue destruction, usually requiring radical surgery and subsequent complex reconstruction. Although breast and penile paraffinomas have been widely described and their management is quite standardized, paraffinomas of the knee are still rare, and only a few case reports or small case series are available in the current literature (Table 1).
CASE
We describe the case of a 77-year-old Caucasian man who was referred to our clinic because of a swollen and painful right knee, skin ulcerations, fistulae, and functional limitation. He denied any history of recent trauma or infections; nonetheless, the patient admitted to the self-injection of paraffin oil 58 years before to treat a subcutaneous defect occurring after a large post-traumatic hematoma. Physical examination revealed dark and hard skin, forming firm plaques (27×21 cm) that involved superficial layers of the anterolateral aspect of the knee; small ulcerations and fistulae secreting purulent exudate were also observed (Fig. 1). The patient reported worsening limitation of the flexion and extension of the right knee during the previous 4 months. Radiological examination revealed soft tissue swelling with several dense and streaky calcifications (Fig. 2). Blood test findings were within normal limits. The patient reported type 1 diabetes and was a heavy smoker.

Right knee upon presentation
The right knee is shown at the time of admission, with dark and hard skin, forming firm plaques and skin ulcerations. Several fistulae secreting purulent exudate were also present.
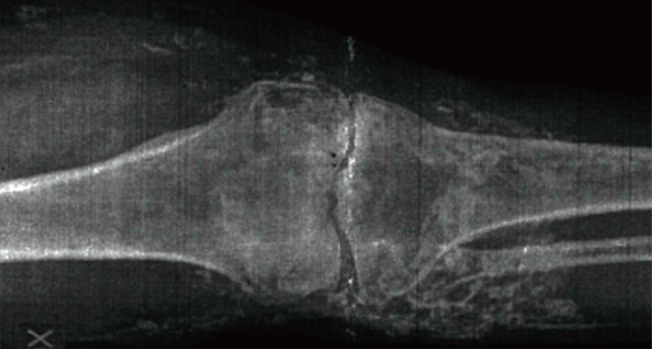
Preoperative radiograph of the right knee
The preoperative radiographic scan of the right knee shows several dense, rounded, and streaky calcifications.
The patient underwent a wide surgical resection of the skin overlying the knee, which was firmly adherent to the joint capsule, and a nearly circumferential, full-thickness excision up to the skeletal muscle in the distal third of the thigh and proximal third of the leg (Fig. 3). As the presence of risk factors such as diabetes and smoking advised against the use of microsurgical techniques, a less invasive two-stage reconstruction using bilayer acellular dermal matrix (IntegraLifeSciences, Plainsboro, NJ, USA) (Fig. 4) and subsequent split-thickness skin grafts (STSG) after 20 days was performed. Histological examination revealed no evidence of any paraffin; nonetheless, dense and fibrous connective tissue with chronic inflammatory cell infiltrate was observed. Several optically empty vacuolar structures surrounded by foreign-body-type multinucleated giant cells were also detected, suggesting an oleo granulomatous reaction to foreign material. Postoperative recovery was uneventful and the patient was discharged 4 days after the second operation. Follow-up after 16 months showed no signs of skin ulcerations or inflammation, with an overall improvement in function (Figs. 5, 6). A range of motion for the right knee from 10° to 100° during active mobilization and from 0° to 110° during passive mobilization was measured (Fig. 7).

Intraoperative photograph of the right knee
Wide surgical excision (27×21 cm) of the soft tissueoverlying the knee was performed.

Application of ADM
Bilayer acellular dermal matrix (IntegraLifeSciences, Plainsboro, NJ, USA) was applied after debridement. ADM, acellular dermal matrix.

Right knee 16 months postoperatively
A photograph of the right knee at 16-month follow-up showing a good anatomical contour of the knee.

Postoperative right knee in flexion
A photograph shows the overall functional improvement with the knee flexed.
DISCUSSION
Although paraffin oil injection has been abandoned as of several decades ago, severe long-term complications may still be encountered in clinical practice. As spontaneous regressions of paraffinomas have not been reported, the only recommended therapy usually consists of complete removal of the affected skin and subsequent reconstruction. Breast paraffinoma is a well-described complication of paraffin oil injection for breast augmentation and its management mainly consists of subcutaneous mastectomy with implant or a myocutaneous flap reconstruction. Reconstruction after penile paraffinoma often requires skin grafts or bilateral scrotal flaps [2].
Paraffinoma of the knee is a still rare phenomenon and few cases are recorded in the literature (Table 1). As it usually consists of massive infiltration and destruction of the surrounding tissues, thus compromising the use of available local flaps, its treatment is often challenging. Furthermore, when joints are involved, a dissection plane between the affected tissue and periarticular structures cannot be easily found. Up to now, soft tissue reconstructions after paraffinoma of the knee have been performed by using direct wound closure, or local or free flaps [1234]. We propose a new alternative reconstruction using acellular dermal matrix (ADM) and STSG for a reliable and less invasive procedure. Skin grafts have not been used on joint surfaces in the past due to their high rate of contraction, with substantial morbidity such as restriction of joint mobility, often requiring multiple corrective surgical procedures. Nevertheless, in the last few years it has been demonstrated that the use of an artificial dermis that contains elastin is very effective from a functional and aesthetic standpoint for minimizing contractures and enhancing skin elasticity. Currently, ADM is a standard tool in reconstructive surgery and has been demonstrated to provide pliable and durable skin cover with minimal donor site morbidity or long-term postoperative contractures. The surgical technique and postoperative care are now simpler and the hospital stay is shorter, and indications for the use of ADM products have now widened to include joints [5]. ADM seems to be a safe and reliable alternative to free tissue transfer in elderly patients with several comorbidities, thus allowing challenging soft tissue reconstructions even in a compromised host.
Soft tissue reconstruction after paraffinoma of the knee can be very complex, due to the paucity of local available tissues and the functional relevance of this area. Furthermore, as paraffin oil injection is an obsolete procedure, these lesions are usually diagnosed as late complications in elderly patients who may present multiple medical problems; in that case, free tissue transfer can be associated with elevated rates of perioperative morbidity and mortality. Thus, ADM seems to be a safe, reliable and simple tissue-engineered alternative for challenging reconstructions that require a large amount of soft tissue.
To our knowledge, the present case is the first report of the application of ADM for the management of paraffinoma in an uncommon site such as the knee.
Notes
No potential conflict of interest relevant to this article was reported.