Algorithm for Primary Full-thickness Skin Grafting in Pediatric Hand Burns
Article information
Abstract
Background
Pediatric hand burns are a difficult problem because they lead to serious hand deformities with functional impairment due to rapid growth during childhood. Therefore, adequate management is required beginning in the acute stage. Our study aims to establish surgical guidelines for a primary full-thickness skin graft (FTSG) in pediatric hand burns, based on long-term observation periods and existing studies.
Methods
From January 2000 to May 2011, 210 patients underwent primary FTSG. We retrospectively studied the clinical course and treatment outcomes based on the patients' medical records. The patients' demographics, age, sex, injury site of the fingers, presence of web space involvement, the incidence of postoperative late deformities, and the duration of revision were critically analyzed.
Results
The mean age of the patients was 24.4 months (range, 8 to 94 months), consisting of 141 males and 69 females. The overall observation period was 6.9 years (range, 1 to 11 years) on average. At the time of the burn, 56 cases were to a single finger, 73 to two fingers, 45 to three fingers, and 22 to more than three. Among these cases, 70 were burns that included a web space (33.3%). During the observation, 25 cases underwent corrective operations with an average period of 40.6 months.
Conclusions
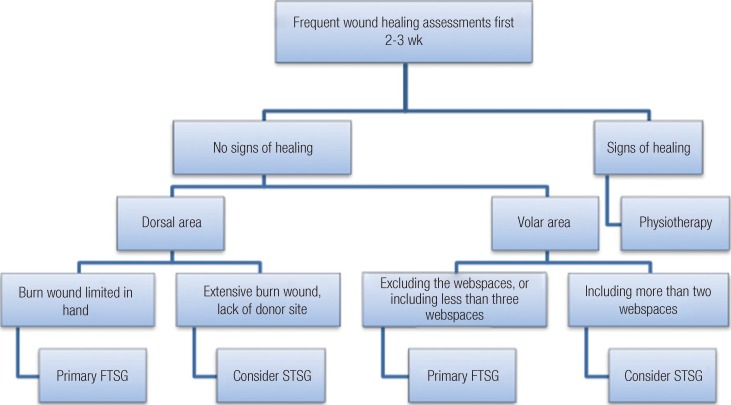
In the volar area, primary full-thickness skin grafting can be a good indication for an isolated injured finger, excluding the web spaces, and injuries of less than three fingers including the web spaces. Also, in the dorsal area, full-thickness skin grafting can be a good indication. However, if the donor site is insufficient and the wound is large, split-thickness skin grafting can be considered.
INTRODUCTION
The surface area of the hand accounts for less than 5% of the total body surface area; however, its functional role is very important, making functional impairment a significant factor for a patient's return to normal social life. The occurrence of hand burns in pediatrics is reported to account for 15% of overall burn cases, which makes these burns quite common [1]. In particular, unlike adult hand burns, pediatric hand burns undergo functional and aesthetic after-effects due to rapid developmental growth during childhood. Therefore, appropriate treatment at an early stage is very important. A surgeon preparing to operate on deep second- or third-degree burns must consider whether to operate using split-thickness skin grafting or full-thickness skin grafting. This study provides a comparative analysis of the existing studies of reconstruction operations carried out over the past 12 years on pediatric hand burn patients who have undergone primary full-thickness skin grafting. This study also included a retrospective analysis of outcomes for patients who underwent full-thickness skin graft at our hospital. The study suggests guidelines for full-thickness skin grafting based on our experience.
METHODS
This study examined 210 patients who visited the hospital due to hand burns and received a full-thickness skin graft from January 2000 to May 2011. All patients were operated on within 2 to 3 weeks after burn injury. After confirming a decrease in inflammation signs (reduced edema, swelling, exudates), skin grafting must be performed after removing suspicious burn wounds including any unstably healed wound margins. All skin grafts were harvested from the inner aspect of the inguinal area to hide the scar exposure. After meticulous bleeding control, each hand axis must also maintain a radial shape and have a maximum skin grafting surface area with web space extension using a K-wire fixing method. We applied a single sheet skin graft as often as possible [2].
The patients' age, gender, the area of hand burn, the number of affected fingers, and the presence of burns on the web space were analyzed. The patients with an average observation period less than 1 year were excluded from this study because revisions were performed at least 1 year after the operation. Post-surgical outcomes were analyzed according to scar contracture formation, the need for reconstruction due to the presence of web deformity, the type of reconstructive surgery, and the time elapsed until reconstruction; the results were compared with those of existing studies. Statistical analysis was performed using Fisher's exact test and Pearson's χ2 test to evaluate the revision rate.
RESULTS
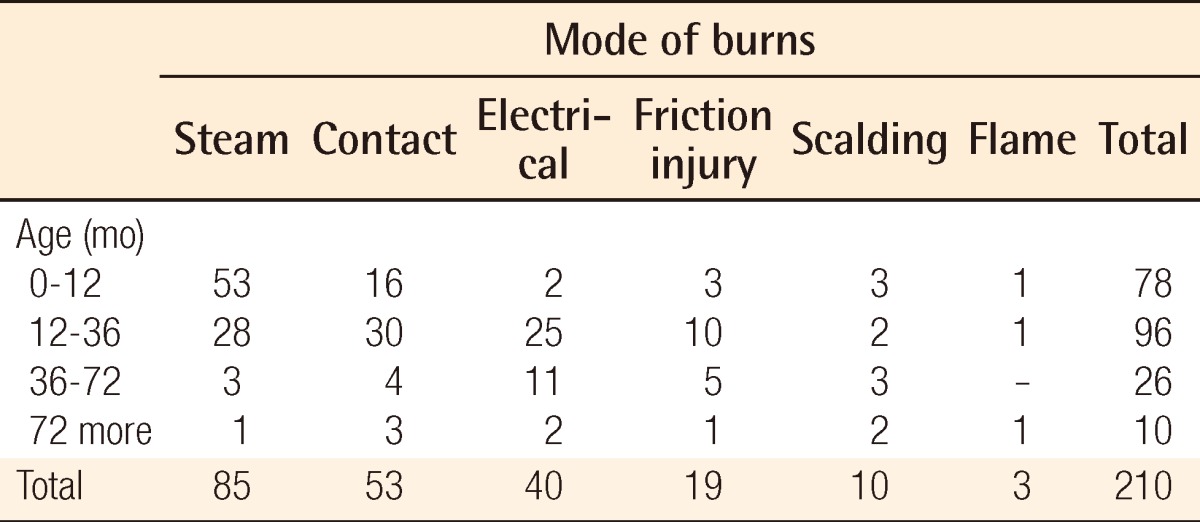
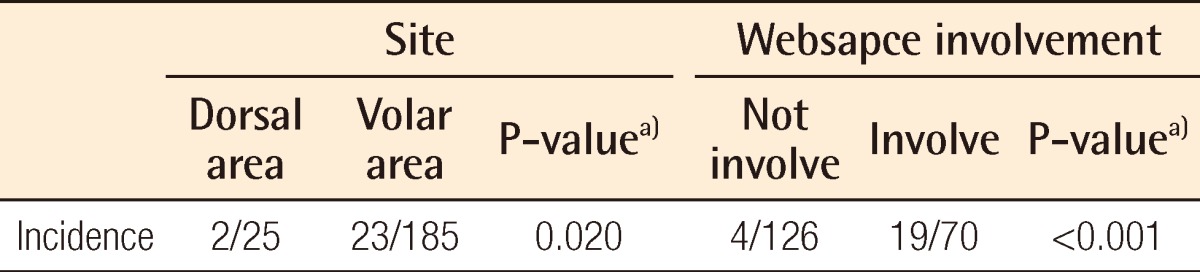
The patients' ages were 8 to 94 months when their respective burns occurred, with an average age of 24.4 months. The patients included 141 males and 69 females. The modes of the burns were as follows: 85 steam burns, 53 contact burns, 40 electrical burns, 19 friction injuries, 10 scalding burns, and 3 flame burns (Table 1). Full-thickness skin grafting was performed in 25 cases on the dorsum of the hand and 185 on the volar area. The number of fingers affected was 56 cases on a single finger, 73 cases on two fingers, 45 on three fingers, and 22 on more than 3 fingers. In total, 70 of these cases involved a web space burn. Nine involved isolated dorsum burns, and 7 involved palmar burns. During the average 6.9-year observation period (1 to 11 years) for the 210 patients, a full-thickness skin graft was re-performed due to scar contracture formation in 5 cases, local flap was performed due to deformity of the web space in 10 cases, and both full-thickness skin grafting and local flap were performed in 10 cases. After the primary full-thickness skin grafting, the average period to revision was 40.6 months (Table 2). The revision rate was higher in cases that included the web space than in the cases that did not include the web space (P<0.001). The revision rate was higher in the volar area than the dorsum area (P=0.020) and was higher in the cases that involved more fingers regardless of the site (P<0.001) (Table 3).
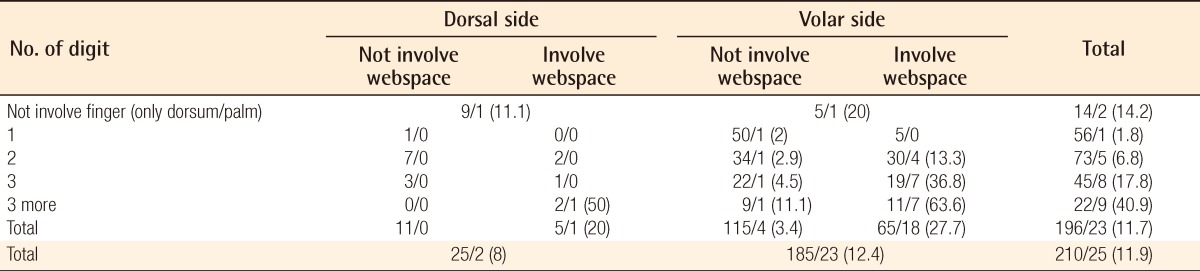
The number of primary full-thickness skin grafting operations and revisions according to the number of digits and sites
Case 1
An 8-month-old male patient visited the hospital due to a steam burn. Necrotic tissue and granulation tissue were observed on the 2nd and 3rd fingers; the web space was not involved. The patient underwent a full-thickness skin graft 20 days after the burn injury, and the skin was harvested from the inner side of the inguinal area. The site showed hyperpigmentation 9 years after the operation, but there were no signs of scar contractures or hypertrophic scars (Fig. 1).

Injury of double digits excluding the web space by rice cooker steam
(A) Nineteen days after the burn injury. Note the presence of necrotic tissue and the unstable marginal wound on the 2nd and 3rd finger. (B) Five days after a full-thickness skin graft. (C) Nine years after the operation. Hyperpigmentation at the site was observed, but no sign of deformity.
Case 2
An 8-month-old female patient visited the hospital due to a steam burn by a rice cooker. A deep second-degree burn was observed, and 15 days after the burn injury, debridement and full-thickness skin graft was performed on the 4th and 5th fingers along with the web space. The skin was harvested from the inner aspect of the inguinal area. The site showed hyperpigmentation 4 years after the operation, but showed no deformity of the web space or motion limitation (Fig. 2).
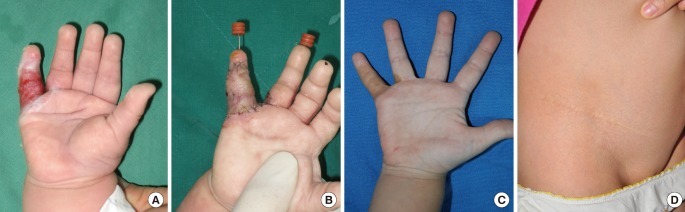
Injury of double digits including the web space by rice cooker steam
(A) Fourteen days after burn injury. (B) Debridement and full-thickness skin graft were performed on the 4th and 5th fingers along with the web space. (C) Four years after the operation. No motional limitation occurred. (D) Long-term outcome of the donor site. The donor scar can be hidden by innerwear.
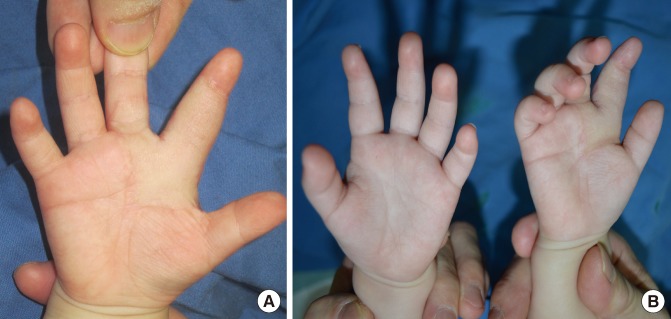
Case 3
A 12-month-old male patient visited the hospital due to a contact burn caused by touching a hot pot lid. Unhealthy granulation tissue formed, and seventeen days after the injury, debridement of the 2nd, 3rd, and 4th fingers, including the web spaces, and full-thickness skin graft was performed. On follow-up, 4 years and 6 months after the operation, contracture was detected due to the deformity of the web space between the second and third finger. A V-M local flap was then performed. Hyperpigmentation was observed 6 years after the burn, but no signs of web space deformity, hypertrophic scarring, or motion limitation were observed (Fig. 3).

Injury of triple digits including the web space in between the digits by a hot pod lid
(A) Sixteen days after burn injury. An unhealthy granulation tissue formed. (B) On follow-up, 4 years and 6 months after primary full-thickness skin graft, a linear contracture band occurred due to the deformity of the web space. (C) Postoperative results of the V-M flap 6 years after the burn injury. No limitation in range of motion interrupting digital abduction occurred.
DISCUSSION
Unlike adult hand burns, pediatric hand burns remain a difficult problem because of the serious risk of hand deformity along with functional impairment due to cicatricial contracture, which results from a patient's rapid growth during childhood. Deciding to perform split-thickness skin grafting or full-thickness skin grafting in the acute phase is always complicated at the time of the burn. Several clinics have suggested that full-thickness skin grafting in an acute pediatric hand burn may cause scarring at the base of the grafting site due to continuous inflammation; hence, a previous study has recommended general wound treatment until the wound remodeling period has ended, and then repair of the cicatricial contracture should be performed [2]. Additionally, in pediatric cases, it is difficult to determine the depth and range of a burn, and to also reach agreement on post-surgery management.
The take rate of full-thickness skin grafts is lower than split-thickness skin grafts because of edema and inflammatory reactions; therefore, consideration is typically given to preserving the donor skin for further full-thickness grafts. However, a recent long-term analysis of pediatric hand burns confirmed that primary full-thickness skin grafting was superior to split-thickness grafts because it reduced the necessity of secondary reconstruction operations, and even if reconstruction was required, full-thickness skin grafting could also delay the duration [3-5]. Therefore, a primary full-thickness skin grafting method and selection of the graft site are important for the preservation of relatively limited donor sites.
To improve the take rate of primary full-thickness skin grafting, surgery should be performed during reduced inflammatory reaction conditions. Surgery performed within 2 to 3 weeks after an injury allows a surgeon to easily determine if the area requires debridement. After 3 weeks, the margin of debridement becomes unclear due to unstable re-epithelization; therefore, because the progress of scar contracture occurs faster in pediatric patients than in adults, postoperative physiotherapy should be performed as soon as possible.
Recently, early excision and skin grafting have been advocated to reduce mortality, duration of illness, and the cost and length of hospital stay. Omar and Hassan [6] had reported that early excision and skin grafting had better results than delayed grafting such as preservation of hand function and shortened hospital stay. Tambuscio et al. [7] reported that early surgical treatment can reduce readmission for secondary revisions. However, unlike adults, in pediatric patients, it is difficult to judge the exact depth and range of excision within 5 days post-burn; even if the operation is performed, graft loss still occurs frequently. A decision well in advance is needed on the preservation of relatively limited skins from donors.
Among the pediatric patients who were treated for acute burn injury without surgery and experienced hand deformation, flexion contracture accounted for 38% of the cases and cicatricial syndactyly accounted for 30% [8]. As a result of long-term observation in our study, cases involving finger reconstruction of the volar side, excluding the web spaces, showed a markedly low revision rate (4/115, 3.4%) (Table 2). Additionally, by performing full-thickness skin grafts, flexion contracture and cicatricial syndactyly did not occur. In other words, primary full-thickness skin grafting is a good indication for volar finger reconstruction, excluding web spaces, regardless of the number of injured fingers.
According to the long-term, 10-year observations on skin grafting such as the study by Chandrasegaram and Harvey [9], scar release operations were performed in 50% of the split-thickness skin grafts used on the volar area. Therefore, primary full-thickness skin grafting is a good choice from a revision rate perspective, even when web spaces are included (18/65, 27.7%, P=0.045). However, in cases where more than 3 fingers are involved, including each web space, determining the appropriate region of debridement is difficult, and occurrence of scar contracture is high due to partial skin loss. Additionally, in our study, full-thickness skin grafting had to be re-performed during revision due to severe webbing deformity. In other words, primary full-thickness skin grafting is not recommended for burns that encompass more than three fingers that include the web spaces.
As reported by Chandrasegaram and Harvey [9], when performing split-thickness skin grafting, the dorsal area had a lower post-surgery contracture rate (4/19, 21%) than the palmar area (8/12, 67%). Split-thickness skin grafting on the dorsum of the hand (4/19, 21%) has been acknowledged as having a higher post-surgery contracture rate than full-thickness skin grafting at the same site (2/25, 8%); however, in cases of large burns that lack a donor site or when donor tissue requires preservation for further full-thickness skin grafting, split-thickness skin grafting on the dorsal area can be considered.
Even primary full-thickness skin grafting cannot avoid deformation of the web spaces. According to our study analysis, cases of burns that included the web space had a higher revision rate (20/70, 28.6%). However, even when a linear scar band that interferes with digital abduction occurs, this can be resolved using Z-plasty or V-M plasty without further skin grafting, and the operation period can be delayed until the deformity has essentially ceased [10].
The main limitation of full-thickness skin grafting is the resulting color difference. In particular, palmar areas, like the soles, consist of a unique type of epidermis and thus show many differences from inguinal skin in properties including texture and hardness. To overcome this problem, our hospital used the lateral aspect of the inguinal area, which markedly reduced the obvious color differences (Fig. 4).
Outcome of skin harvested from the lateral aspect of the inguinal area
(A) Full-thickness skin graft was performed. During the operation, donor skin was taken from the lateral aspect of the inguinal area, and after 6 months, no hyperpigmentation was seen, (B) and the color of the left and right hand was indistinguishable.
The present study concluded that a maximum positive outcome could be obtained by following the below guidelines (Fig. 5): 1) To increase the take rate, a careful and technical debridement is required, and the operation should be performed when the inflammation reaction has decreased. The maximum skin grafting area must be obtained. 2) In the volar area when finger reconstruction excludes the web spaces, full-thickness skin grafting can be an absolute indication. Full-thickness skin grafting on less than 3 fingers including the web spaces may reduce the subsequent reconstruction rate. 3) In the dorsal area when only the dorsal hand area is burned, primary full-thickness skin grafting may be a good procedure to perform. However, if the donor site is insufficient and the wound is large, split-thickness skin grafting on the dorsal area can be considered. 4) Through regular follow-up, web space deformity that interrupts digital abduction can be resolved using a simple local flap. 5) To overcome the color difference, from an aesthetic point of view, donor skin should be obtained from the lateral aspect of the inguinal area.
Notes
No potential conflict of interest relevant to this article was reported.