Innovation in the planning of V-Y rotation advancement flaps: A template for flap design
Article information
Abstract
Local flaps exhibit excellent color matching that no other type of flap can compete with. Moreover, surgery using a local flap is easier and faster than surgery using a distant or free flap. However, local flaps can be much more difficult to design. We designed 2 templates to plan a V-Y rotation advancement flap. The template for a unilateral V-Y rotation advancement flap was used on the face (n=5), anterior tibia (n=1), posterior axilla (n=1), ischium (n=1), and trochanter (n=2). The template for a bilateral flap was used on the sacrum (n=8), arm (n=1), and anterior tibia (n=1). The causes of the defects were meningocele (n=3), a decubitus ulcer (n=5), pilonidal sinus (n=3), and skin tumor excision (n=10). The meningocele patients were younger than 8 days. The mean age of the adult patients was 50.4 years (range, 19–80 years). All the donor areas of the flaps were closed primarily. None of the patients experienced wound dehiscence or partial/total flap necrosis. The templates guided surgeons regarding the length and the placement of the incision for a V-Y rotation advancement flap according to the size of the wound. In addition, they could be used for the training of residents.
INTRODUCTION
Local flaps exhibit excellent color matching that no other type of flap can compete with. Moreover, surgery using a local flap is easier and faster than surgery using a distant or free flap. When planning a flap, the surgeon must consider the size, mobility, viability, and donor area of the flap. Performing more extensive incisions to increase the mobility of the flap decreases its blood perfusion. Harvesting a flap larger than is needed may help to close the defect, but it jeopardizes the primary closure of the donor area. After having reviewed the literature, we incorporated findings from previous research with our experiences [1,2] to develop an optimal geometrical formula for unilateral and bilateral V-Y rotation advancement flaps [3]. According to the formula, we designed 2 templates (patent pending) for flap planning. The templates guide surgeons about the size of the required flap for defects of any size, to the extent allowed by the adjacent tissues.
IDEA
Design of the template
According to a previous review, the length of a unilateral V-Y rotation advancement flap is equal to 3 times the horizontal radius (r) of the defect (BC=3r). The length of the bilateral V-Y rotation advancement flap is equal to twice the radius (BC=2r) [3]. We realized that keeping the corner of the flap straight rather than curved facilitated the closure of the donor area and saved more tissue. Therefore, the corner of the flap is made of an isosceles triangle without a base (DCE), and the height of this imaginary triangle equals the radius of the defect (Fig. 1).
Mathematical illustration of the templates
Illustration of the mathematical equations for the design of unilateral and bilateral V-Y rotation advancement flaps.
The template is made of stainless steel. However, it can be constructed from any flexible and sterilizable material. The template has multiple loops that allow flaps to be designed for different defect sizes. The distance FF′ equals the diameter of the wound. The template for bilateral V-Y rotation advancement flap is made of 9 loops with dimensions (FF′×CC′) ranging from 2×6 to 10×30 cm. The template for unilateral V-Y rotation advancement flap is made of 14 loops with dimensions (FF′×AC) ranging from 2×4 to 15×30 cm. The template has longitudinal and oblique stalks. At the intersection of these stalks, there is a hole that determines the center of the template. In order to design the flap, the center of the flap should overlap with the center of the tissue defect. After considering the relaxed skin tension lines and deciding the orientation of the flap, the template is placed on the defect. The smallest loop that tangentially (points F and F′) covers the edges of the wound dictates the size of the flap that should be used. The flap is then drawn with a skin marker from the longitudinal stalk to the oblique stalk. The oblique stalk indicates the end of the back-cut; thus, the drawing should be stopped when the marker hits the oblique stalk (Fig. 2).
Patient no. 19, with meningocele
(A) A meningocele defect measuring 4×3.5 cm. (B) The template for the bilateral flap was centered on the defect. The third loop of the template was chosen according to the size of the defect. (C) The flaps were dissected in the supramuscular plane and completely freed from the floor. (D) Photograph taken 2 weeks postoperatively.
For example, for a defect with a diameter of 2 cm, the smallest loop of either the bilateral or unilateral template should be used. For a bilateral V-Y rotation advancement flap, the distance between the center of the wound (A) and the corner of the flap (C) is 3 cm (distance between C and C′: 6 cm); however, for unilateral V-Y rotation advancement flap, the corresponding distance would be 4 cm.
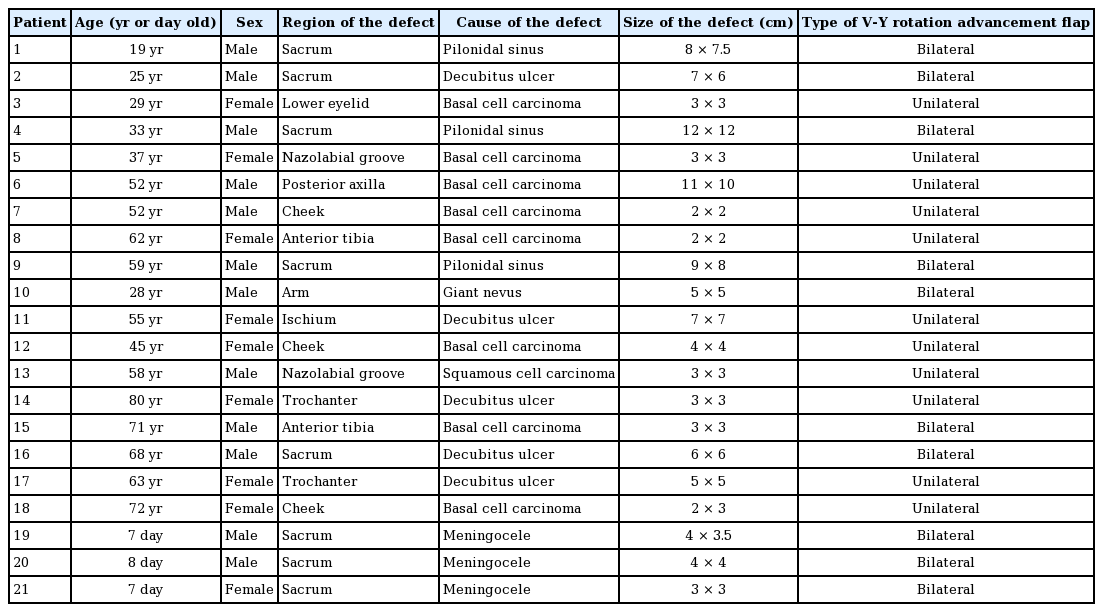
Case series
Twenty-one patients were operated on with the help of the template. The causes of the defects were meningocele (n=3), a decubitus ulcer (n=5), pilonidal sinus (n=3), and excision of a skin tumor (n=10). The patients with meningocele were younger than 8 days. The mean age of the adult patients was 50.4 years (range, 19-80 years). The template for a unilateral V-Y flap was used on the face (n=6), anterior tibia (n=1), posterior axilla (n=1), ischium (n=1), and trochanter (n=2) (Fig. 3). The template for a bilateral V-Y rotation advancement flap was used on the sacrum (n=8), arm (n=1), and anterior tibia (n=1). The size of the defect ranged from 2×2 to 11×10 cm for the unilateral flaps and 3×3 to 12×12 cm for the bilateral flaps. The details of the patients are presented in Table 1. All the flaps were raised above the superficial fascia or superficial muscular aponeurotic system. All the donor areas of the flaps were closed primarily. Patients received prophylactic antibiotics before surgery. Patients with meningocele or a decubitus ulcer received antibiotics for 5 days after the surgery. All the patients were followed for at least 6 months. No complications such as wound dehiscence, infection, hematoma, or partial or total flap loss occurred.
Patient no. 18, with basal cell carcinoma
(A) The tumor was excised and a defect measuring 2×3 cm was created. (B) A unilateral flap was planned and second loop of the template was chosen according to the size of the defect. (C) Photograph taken 2 months postoperatively. A good aesthetic result was obtained, with an inconspicuous scar.
DISCUSSION
Surgeons plan flaps according to their experience. There is no generally accepted mathematical rule that describes the dimensions of the flap relative to the size of the tissue defect. Since there is no quantitative way to explain how to plan a flap, it is not easy to teach this skill to residents in training or other surgeons. In particular, surgeons who do not perform these procedures regularly may be reluctant to operate because of potential complications such as incomplete closure of the defect or flap loss.
The history of plastic surgery is rich in innovations [4]. In order to quantify the design, and to standardize and to facilitate surgery, plastic surgeons have invented different templates or rulers for the Limberg flap [5], Z-plasty [6], facial flap transfer [7], transverse rectus abdominis myocutaneous flap design [8], shaping the free fibula flap [9], complicated syndactyly [10], cartilage shaping in rhinoplasty [11], and breast reduction [12]. The Wise pattern [13] and areola cutter, used in breast reduction, are widely used templates that are commercially available. None of these templates are necessary; however, they allow surgeons to avoid making unnecessary measurements and provide reproducible results.
The templates for V-Y rotation advancement flap help surgeons to plan the flap without worrying whether its size will be sufficient for defect closure. Moreover, it facilitates primary closure of the donor area without compromising the viability or mobility of the flap. Since the surgeon does not need to plan the flap, the operative time can be reduced. In particular, it prevents possible hesitation about how to draw and where to place the back-cut. In addition, keeping the corner of the flap straight rather than curved provides a less bulky appearance and a more aesthetically appealing scar. Since the template provides the optimal ratio of blood supply to flap size, we have not experienced any wound problems, not even delayed healing. However, those templates cannot be used on the scalp, the foot sole, the palm, or previously damaged tissue (due to a burn or radiation injury), where the skin is less elastic than usual.
Those templates enable worry-free V-Y rotation advancement flap design by guiding the surgeon about the length and the localization of the incision according to the size of the wound.
Notes
No potential conflict of interest relevant to this article was reported.
PATIENT CONSENT
The patient provided written informed consent for the publication and the use of their images.