Usefulness of Intravenous Anesthesia Using a Target-controlled Infusion System with Local Anesthesia in Submuscular Breast Augmentation Surgery
Article information
Abstract
Background
Patients have anxiety and fear of complications due to general anesthesia. Through new instruments and local anesthetic drugs, a variety of anesthetic methods have been introduced. These methods keep hospital costs down and save time for patients. In particular, the target-controlled infusion (TCI) system maintains a relatively accurate level of plasma concentration, so the depth of anesthesia can be adjusted more easily. We conducted this study to examine whether intravenous anesthesia using the TCI system with propofol and remifentanil would be an effective method of anesthesia in breast augmentation.
Methods
This study recruited 100 patients who underwent breast augmentation surgery from February to August 2011. Intravenous anesthesia was performed with 10 mg/mL propofol and 50 µg/mL remifentanil simultaneously administered using two separate modules of a continuous computer-assisted TCI system. The average target concentration was set at 2 µg/mL and 2 ng/mL for propofol and remifentanil, respectively, and titrated against clinical effect and vital signs. Oxygen saturation, electrocardiography, and respiratory status were continuously measured during surgery. Blood pressure was measured at 5-minute intervals. Information collected includes total duration of surgery, dose of drugs administered during surgery, memory about surgery, and side effects.
Results
Intraoperatively, there was transient hypotension in two cases and hypoxia in three cases. However, there were no serious complications due to anesthesia such as respiratory difficulty, deep vein thrombosis, or malignant hypertension, for which an endotracheal intubation or reversal agent would have been needed. All the patients were discharged on the day of surgery and able to ambulate normally.
Conclusions
Our results indicate that anesthetic methods, where the TCI of propofol and remifentanil is used, might replace general anesthesia with endotracheal intubation in breast augmentation surgery.
INTRODUCTION
Breast augmentation surgery is commonly performed under general anesthesia with endotracheal intubation or manually controlled intravenous anesthesia. Although surgeons perform the procedure comfortably on patients under general anesthesia, patients have anxiety over complications due to general anesthesia [1]. On the other hand, there are disadvantages in manually controlled infusion including inefficient control of anesthesia [2].
Through development of instruments and introduction of new drugs, various means of anesthesia for breast surgery have been reported [3-5]. More frequent use of a local anesthetic combined with some form of intravenous sedation in office-based facilities has been reported [6-8]. This change keeps hospital costs down as well as saving time for patients.
Propofol, midazolam, and ketamine are most often used for this type of anesthesia. Of these, propofol is characterized by a short onset of action and a prompt recovery from anesthesia. Additionally, in maintaining an appropriate level of sedation, it is necessary to maintain the serum level of drugs through a continuous administration of drugs rather than an intermittent one. The target-controlled infusion (TCI, Ochestra Base Primea, Fresenius Kabi Company, Brezins, France) system can administer drugs to patients more precisely and consistently. Propofol is used for the hypnotic effect, and local anesthesia or analgesic agents are used for pain control.
We conducted this study to assess whether intravenous anesthesia using the TCI system with propofol and remifentanil would be an effective method of anesthesia in breast augmentation surgery.
METHODS
This retrospective study included 100 consecutive patients who had recently undergone breast augmentation using a TCI of propofol and remifentanil from February to August 2011. Patient selection was limited to patients who met the American Society of Anesthesiologists class I or II criteria for medical history taking and physical examination. All the patients were examined for the total operation time, the total dose of drugs administered during surgery, memory of their surgery, and complications.
Patients were hospitalized after fasting from clear liquids for 2 hours, from milk for 4 hours, and from meat for 6 to 8 hours prior to the surgery. The patients were also given an intramuscular injection of 0.1 mg of glycopyrrolate 30 minutes prior to surgery, and 3 L/min O2 was supplied to the patients via a nasal cannula. In all of the patients, the oxygen saturation and the electrocardiography pulse rates were continuously measured during surgery. Respiratory status was monitored and blood pressure was measured at 5-minute intervals. At the start of surgery, we induced anesthesia using a bolus injection of 0.05 mg/kg of midazolam and 1 mg/kg of ketamine.
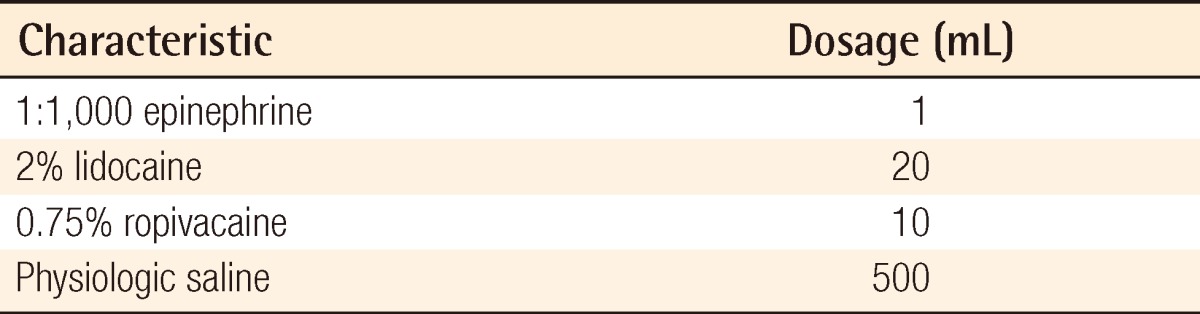
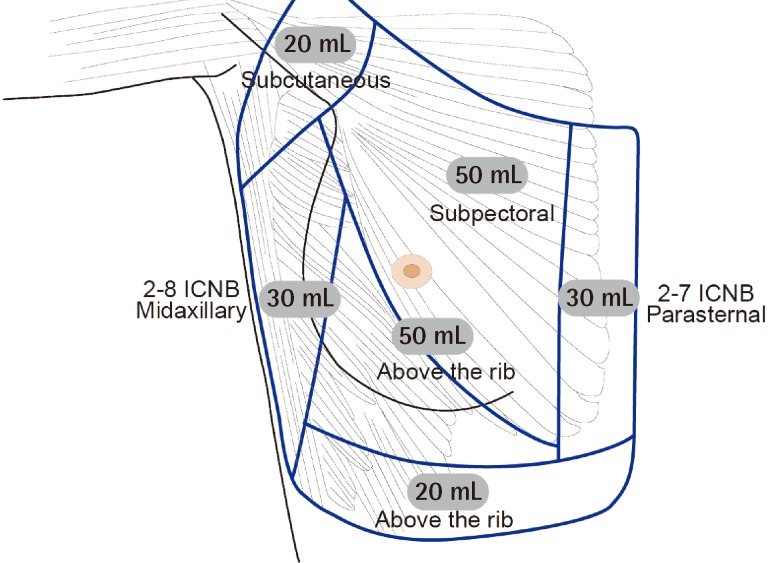
When the patients demonstrated relaxation and slurred speech, we initiated local anesthesia. Local anesthesia was performed using a mixture of 1:1,000 1 mL of epinephrine, 20 mL of 2% lidocaine, 10 mL of 0.75% ropivacaine in a 500 mL saline solution (Table 1). We performed an intercostal nerve block in a range extending from the 2nd to 8th intercostal nerve on the mid-axillary and 2nd to 7th intercostal nerve on the parasternal area. The intercostal nerve block was performed with a 24 gauge×19 mm needle contacting the bone perpendicularly at the mid-portion of the ribs. The tip was then moved to the lower one-third part, and 2 to 3 mL of local anesthetics was injected. Consequently, we could prevent pneumothorax and possible neurovascular injuries, which would have originated from the direct local anesthetic injection into the intercostal neurovascular bundles. We injected local anesthetics using a 21 gauge×89 mm spinal needle to the subpectoral area in the breast, above the rib, and subcutaneous tissues on the axilla (Fig. 1).
The patients were given an injection of 10 mg/mL propofol (Anepol, HaNa Pharm, Seoul, Korea) using a TCI system 10 to 15 minutes following local anesthesia. The pharmacokinetic model was based on that of Schnider et al. [9]. The initial effect-site target concentration of propofol was set at 2 µg/mL. After the concentration of propofol reached the target level, 50 µg/mL of remifentanil (Ultiva; GlaxoSmithKline, Parma, Italy) was infused using a TCI system; this was based on the Minto model [10]. The target concentration was adjusted to 2 ng/mL.
We performed an incision when the concentration of propofol and remifentanil reached 2 µg/mL and 2 ng/mL, respectively. Surgery was performed via a transaxillary approach. A skin incision was made only up to the subcutaneous layer. Meanwhile, the pocket was made subpectorally. To minimize the patients' pain, an incision was performed mainly using a scalpel. For hemostasis, a bipolar cautery was used.
We titrated the effect-site concentration of propofol and remifentanil against its clinical effects and vital signs. The target concentration was adjusted depending on the severity of pain. In cases that were predicted to have serious pain including from incision and dissection of the pocket, we increased the dosage of propofol in advance. The target level of the concentration was adjusted in a way that patients could have spontaneous respiration. In addition, we ensured that the vital signs of the patients were within 20% of the baseline of each patient. From 10 minutes before the completion of the surgical procedure, the TCI system for remifentanil was adjusted to 0 ng/mL. The TCI system for propofol was then lowered to 0 µg/mL. Thus, the plasma concentration of the drugs was gradually decreased (Fig. 2).
Following the completion of the surgical procedure, the blood pressure and oxygen saturation were measured. Once the patients became alert, they were transferred to a recovery room. There they were continuously monitored for at least an hour until meeting discharge criteria [11]. Unless patients had symptoms such as vomiting, they were immediately allowed oral intake beginning with water. They were also allowed to undergo ambulatory movement to a restroom in the recovery room. The patients were advised not to drive their cars for at least the next 24 hours after they regained consciousness. They were discharged with their caregivers who could take care of them on the day of surgery.
RESULTS
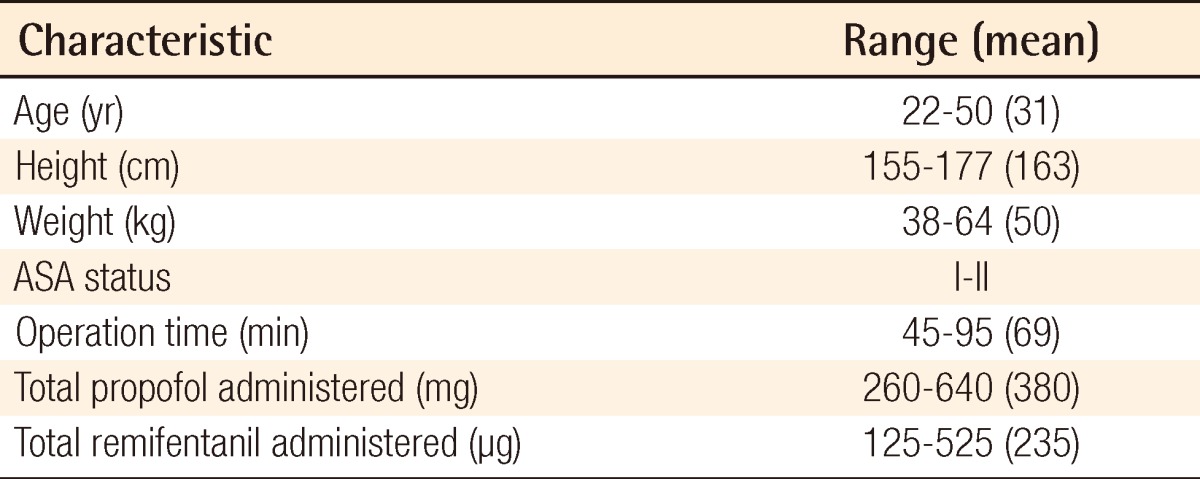
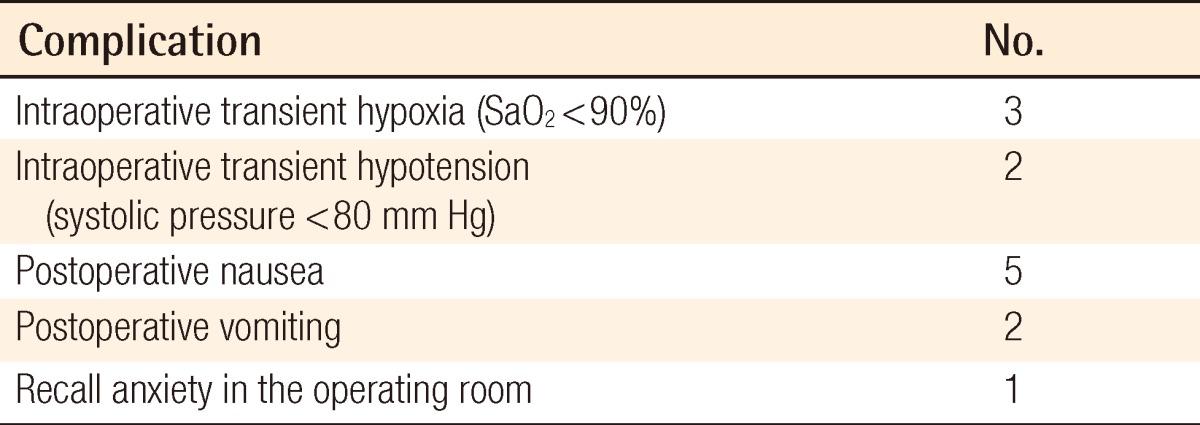
In our clinical series of patients, the mean age was 31 years (range, 22 to 50 years), the mean height was 163 cm, and the mean weight was 50 kg. On review of past history, there were no notable diseases. The mean operation time was 69 minutes. The mean amount of propofol and remifentanil, which were intraoperatively administered, was 380 mg (range, 260 to 640 mg) and 235 µg (range, 125 to 525 µg), respectively (Table 2). Intraoperatively, there were two cases in which the systolic pressure was transiently changed to ≥150 mm Hg or ≤80 mm Hg; these were easily managed with fluid therapy or the adjustment of anesthetic agents. In addition, there were no cases in which an endotracheal intubation was needed. In three patients, there was transient respiratory depression where the oxygen saturation was lowered to ≤90, but these cases were managed immediately by decreasing the anesthetic dosages, elevating their chins, maintaining the airway, and chest wall compressions or surgical stimuli. Postoperatively, there were five cases of mild nausea and two cases of vomiting; these cases were resolved without medication. There was no clear memory of the intraoperative events, but one patient had an obscure memory about them (Table 3). All of the patients achieved prompt recovery with postoperative discontinuation of drugs, and they were able to ambulate for themselves. The length of stay in the recovery room was from 1.2 to 5 hours (mean, 2.5 hours). All the patients were discharged on the day of surgery and were able to normally ambulate for themselves.
DISCUSSION
Patients have reservations regarding general anesthesia due to fear of complications. This has led to greater use of total intravenous anesthesia for breast augmentation surgery. This type of anesthesia has some advantages over general anesthesia with endotracheal intubation such as having none of the side effects associated with inhalation anesthetic agents that are used in general anesthesia. Moreover, because patients have mobility under total intravenous anesthesia, deep vein thrombosis might not occur at all, and the expenditure on anesthesia can be reduced. In addition, the time spent on the induction of anesthesia and endotracheal intubation can also be reduced.
The use of anesthetic agents with prompt action and a short half-life would be both more convenient and safer for performing a surgical procedure under intravenous anesthesia [12]. The intravenous anesthetics that are commonly used in a clinical setting are benzodiazepine, propofol, barbiturate, opioid, ketamine, and β-2 agonist. Considering the overall status of patients, the types and scope of surgery, and the severity of pain, these anesthetics might be used solely or concomitantly. In particular, propofol is a sedative that is commonly used. A 3-compartment model study showed that the initial distribution half-life of propofol is approximately 2 to 4 minutes [13]. The effects of sedation and anesthesia are seen 40 seconds after administration. Even after prolonged administration, patients recover rapidly [13]. Several studies have reported that it causes a lower incidence of nausea and vomiting following surgery [14,15].
Local anesthesia might insufficiently control pain. In these cases, opioid can be infused. Remifentanil is a recently introduced opioid that is an analgesic substance that acts on the µ receptors. It is promptly degraded by the action of non-specific esterase present in the plasma and tissue. Approximately 4 minutes elapses until the plasma level of remifentanil decreases by 50% after its infusion has been terminated following a long-term infusion. It is therefore characterized by a lack of deposition despite repeated dosing or long-term infusion [16]. In particular, if remifentanil is concomitantly used with propofol, it undergoes an independent pathway from propofol [17]. Moreover, compared with other types of opioid, remifentanil has hemodynamic stability during most of the surgical procedure [18].
If drugs are administered for the purpose of performing total intravenous anesthesia, the continuous administration of drugs rather than the intermittent administration of drugs helps to maintain the plasma level of drugs above a certain level of concentration and thereby to keep the sedative effects optimal. In particular, TCI is a system for administering drugs continuously at a dose that has been calculated using a computer based on the status of the patient and the pharmacokinetic characteristics of the drugs to ensure that the theoretical target concentration is maintained. The major benefits of this approach are that clinicians can take immediate measures against an inappropriate depth of anesthesia without any complicated mathematical calculations.
The clinical application of TCI was first introduced by Schwilden and Schuttler [19] in 1990. Since then, it has been developed into the current type of TCI system such that the methods of infusion based on the pharmacokinetic profile can be selected using software. It has already had pharmacokinetic parameters for various types of drugs installed. It has been designed to infuse drugs to achieve a level of concentration at the target sites as well as the plasma concentration. A recent study has shown that the degree of hemodynamic stability was higher following the use of TCI than after the manual administration of remifentanil [20].
As described here, while maintaining a relatively accurate level of the plasma concentration with the use of a TCI system, the depth of anesthesia can be simply adjusted. This establishes an environment where surgeons can concentrate on the surgical procedure. However, monitoring and management of patients should be performed with the same level of attention as is paid during general anesthesia. Patients can be abruptly converted from minimal sedation to a deep level. This might also lead to respiratory depression, hypoxia, and pulmonary aspiration. Meticulously monitoring patients is therefore mandatory. Finally, the status of consciousness should be appropriately evaluated. For the evaluation of a patient's state of consciousness, clinical parameters should be used. It can also be evaluated using objective parameters based on electrophysiologic methods such as the bispectral index [6].
Our results showed some of the patients showed involuntary movement to some extent depending on the magnitude of intraoperative pain or each patient's sensitivity to pain. The time of the persistent presence of stimuli was relatively short. Additionally, the range of motion was limited. Accordingly, there were no interferences with the surgical procedure.
The limitation of the current study is that no cost-effectiveness analysis was attempted. Several studies have explained that anesthesia using propofol and remifentanil is more expensive than other anesthetic methods [21,22]. Considering the medical personnel and equipment associated with anesthesia, however, it would be more cost-effective to use these drugs than traditional anesthesia; this deserves further study.
In conclusion, the following matters should be considered in performing safe surgery under total intravenous anesthesia using the TCI system: 1) A patient's choice is a key factor. Most of the patients who are in need of breast augmentation correspond to the American Society of Anesthesiologists status I or II group. 2) Surgeons should be familiar with the drugs that are used for anesthesia; that is, they should be aware of the variability of intravenous anesthetics and their side effects. 3) In emergency situations, surgeons should use equipment to maintain the airway. Thus, appropriate measures should be taken against hemodynamic derangements such as the abrupt occurrence of respiratory insufficiency and hypotension. A patient's safety should be the first priority, even over cost effectiveness. Therefore, a thorough medical history and physical examination should be performed for each patient. Backup support of anesthesiologists or experienced medical practitioners is also needed as well as an adequate patient transfer system to inpatient hospitals. The anesthetic techniques presented in this paper may require the help and supervision of an anesthesiologist at first.
A retrospective analysis of our clinical series of patients suggests that anesthetic methods under total intravenous anesthesia based on the TCI system using propofol and remifentanil are more convenient than manually controlled infusion and the procedure might replace general anesthesia with endotracheal intubation in breast augmentation surgery.
Notes
This study was supported by Yeungnam University grants in 2011.
This article was presented at the 30th International Meeting of the Korean Society for Aesthetic Plastic Surgery and 10th the Korean Association of Plastic Surgeons on April 13-15, 2012 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.