Basal Cell Carcinoma
Article information
LEARNING OBJECTIVES
After reviewing this article on basal cell carcinoma, the reader should be able to
Review the epidemiology and causes
Describe the common clinical findings and classification
Describe treatment methods
Discuss the prognosis
EPIDEMIOLOGY
Basal cell carcinoma (BCC) is the most common type of skin cancer (75% to 80%) and the most common of all cancers (more than one out of every three new cancers). Seventy to eighty percent of BBC occurs in the head and neck region, followed by the trunk (about 25%), and penis, vulva, or perianal skin (about 5%). It is more common in light-skinned individuals (type 1 or type 2 skin) with a family history of BCC and increases in incidence closer to the equator or at higher altitudes. Incidence is relatively low in Asians, Blacks, and Hispanics. The current male-to-female ratio is approximately 2.1:1. BCC incidence increases with age; about 5% to 15% of BCC cases occur in patients aged 20 to 40 years, and the incidence is more than 100-fold in persons aged 55 to 70 years than in those aged 20 years or younger. BCC accounts for about 0.1% to 2% of all patient deaths due to cancer [1].
CAUSES
BCC is usually caused by a combination of cumulative ultraviolet (UV) light exposure and intense, occasional UV exposure, and overexposure to X-rays or other forms of radiation. BBC also occurs in association with basal cell nevus syndrome, xeroderma pigmentosum, albinism, epidermodysplasia verruciformis, Gardner's syndrome, and nevus sebaceous. Patients receiving immunosuppression therapy are at increased risk for BCC. BBC occurrence in scar tissue has also been reported [2,3].
PATHOPHYSIOLOGY
Basal cell carcinomas develop in the basal cell layer of the epidermis. Exposure to sunlight may cause DNA damage (thymine dimer formation). While DNA repair removes most UV-induced damage, not all cross-links are excised. Thus, cumulative DNA damage occurs. Apart from the mutagenesis, sunlight decreases immune surveillance for new tumor cells [4].
A gene commonly found to be mutated in BCC is the PTCH gene. A PTCH gene mutation at chromosome 9q22.3, which inhibits the hedgehog signaling pathway, is found in patients with basal cell nevus syndrome (Gorlin syndrome). Similarly, a mutation in the SMO gene (hedgehog pathway) also causes basal cell carcinoma [5].
CLINICAL FEATURES
The most commonly found clinical feature of BCC is an elevated tumor with a pearly and translucent margin and telangiectasia. The color may vary widely from nearly normal skin color to erythematous to violaceous and may also be pigmented. BCC may also resemble noncancerous skin conditions such as eczema or psoriasis. The majority of these cancers occur on areas of skin that are regularly exposed to sunlight or other ultraviolet radiation. They may also appear on the scalp [6].
CLASSIFICATION
Basal cell carcinoma has many clinical forms and is commonly classified into the following types [7]:
- Nodular basal cell carcinoma (classic BCC) (Fig. 1): most common type (50% to 80%) and occurs most often on sun-exposed areas of the head and neck (85% to 90%).
- Cystic basal cell carcinoma (Fig. 2): characterized by dome- shaped, blue-gray cystic nodules.
- Morphoeic, morpheaform or cicatricial basal cell carcinoma (Fig. 3): 2% to 6% of BBCs; aggressive variant with distinct white sclerotic plaque and histological appearance.
- Infiltrative basal cell carcinoma (Fig. 4): aggressive type characterized by deep infiltration.
- Micronodular basal cell carcinoma: not clinically distinc tive, histologically micronodular growth pattern, curettage not indicated.
- Superficial basal cell carcinoma (superficial multicentric basal cell carcinoma) (Fig. 5): at least 15% of BBCs; occurs most commonly on the trunk (40%) or distal extremities (14%) and grossly is an erythematous patch similar to ec zema or psoriasis; may grow to a large diameter and is the most common type of BCC in HIV patients.
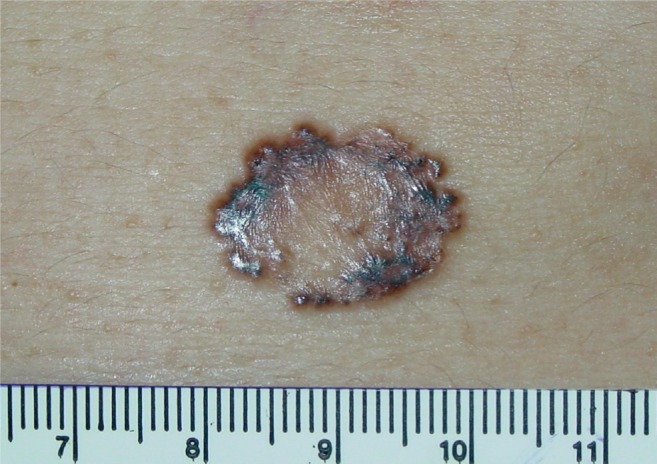
- Pigmented basal cell carcinoma (Fig. 6): about 6% of all BCCs; similar in appearance to nodular BBC but with increased melanization (brown or black); common type of BCC in Asians.
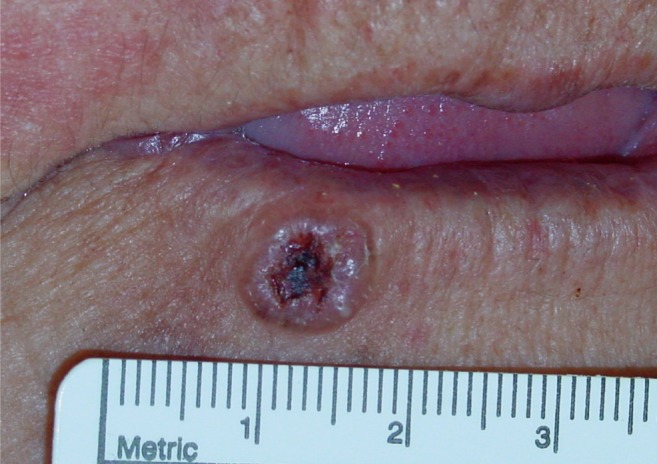
- Rodent ulcer (Jacobi ulcer) (Fig. 7): untreated BCC that has formed ulceration.
- Fibroepithelioma of Pinkus (Fig. 8): most commonly occurs on the lower back, groin, or thigh areas; may grow to large size.
- Polypoid basal cell carcinoma (Fig. 9): characterized by exophytic nodules on the head and neck.
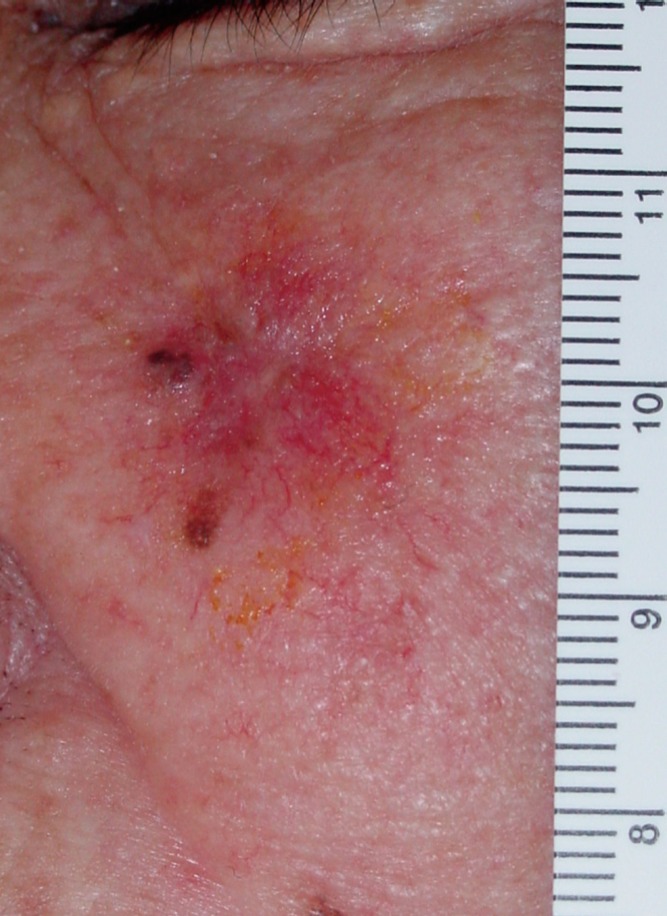
- Pore-like basal cell carcinoma (Fig. 10): usually found in thick sebaceous skin (nose, nasolabial fold, or lower fore head) and resembles an enlarged pore or stellate pit; gener ally in men and the majority are smokers.
- Aberrant basal cell carcinoma: absence of any apparent carci nogenic factor or occurring in odd sites such as the scrotum, vulva, perineum, nipple, or axilla.
- Solitary basal cell carcinoma in the young: occur in the region of facial embryonic clefts and are commonly deeply invasive.
STAGING
Basal cell carcinoma metastasis is very rare; however, the American Joint Committee on Cancer's TNM system is the system most often used for staging [8].
Primary tumor (T)*.
- TX: primary tumor cannot be assessed.
- T0: no evidence of primary tumor.
- Tis: carcinoma in situ.
- T1: carcinoma less than 2 cm in greatest dimension, with less than 2 high-risk features.**
- T2: carcinoma greater than 2 cm in greatest dimension, or a tumor of any size with at least 2 high-risk features.**
- T3: tumor invasion of the maxilla, mandible, orbit, or temporal bone.
- T4: tumor invasion of the skeleton (appendicular or axial) or with perineural involvement of the skull base.
*Excludes cutaneous squamous cell carcinoma of the eyelid.
**High-risk features for the primary tumor (T) staging:
Depth/invasion: >2 mm thickness, Clark level>IV, Peri neural invasion.
Anatomic location: primary site ear, primary site non-hair-bearing lip.
Differentiation: poorly differentiated or undifferentiated.
Regional lymph nodes (N).
- NX: regional lymph nodes cannot be assessed.
- N0: no regional lymph node metastasis.
- N1: metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension.
- N2: metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension; or in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension; or in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension.
- N2a: metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension.
- N2b: metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension.
- N2c: metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension.
- N3: metastasis in a lymph node, more than 6 cm in great est dimension.
Distant metastasis (M)
- M0: no distant metastasis.
- M1: distant metastasis.
Anatomic stage/prognostic groups.
- Stage 0 Tis, N0, M0
- Stage I T1, N0, M0
- Stage II T2, N0, M0
-
- Stage III T3, N0, M0
T1 to T3, N1, M0
-
- Stage IV T1 to T3, N2, M0
T any, N3, M0
T4, N any, M0
T any, N any, M1
TREATMENT
A biopsy should be performed in all lesions suspicious for BCC. The following are common methods used in the treatment of BCC: wide excision, curettage and electrodessication, Mohs micrographic surgery, cryosurgery, and radiation, while topical skin creams with imiquimod or 5-fluorouracil may be used to treat superficial basal cell carcinoma [9].
- Mohs micrographic surgery: single most effective technique for removing BCC.
- Wide excision: the standard surgical margins are 2 to 5 mm when previously untreated and about 1 cm or more for recur rent or large tumors. A frozen biopsy is mandatory to confirm sufficient tumor-free margins.
- Curettage and electrodessication: contraindicated for re current BCC.
- Cryosurgery: not recommended for large and recurrent tumors; less commonly used today.
- Radiotherapy: inoperable or recurrent tumors; for elderly and patients in poor health; contraindicated in the retreat ment of recurrent tumors following previous radiotherapy.
- Topical medications imiquimod or 5-fluorouracil: US FDA-approved for only superficial BCC, cure rate about 80% to 90%.
PROGNOSIS
The 5-year recurrence rates for primary (previously untreated) BCCs are: surgical excision, 10.1%; radiotherapy, 8.7%; curettage and electrodessication, 7.7%; cryotherapy, 7.5%; all non-Mohs modalities, 8.7%; and Mohs micrographic surgery, 1%. Recurrences usually occur 4 to 12 months after initial treatment, and the risk of developing a second lesion in 3 years is about 44%, which is a 10-fold increase over that of the general population [10,11]. Tumors on the nose or T-zone of the face have a higher incidence of recurrence. Recurrence is most common on the nose and nasolabial fold. Infiltrative, micronodular, and multifocal types have higher rates of recurrence than nodular types. Basal cell carcinoma rarely metastasizes (0.028% to 0.55%). The most common sites of metastasis are the lymph nodes, lungs, and bones. Patients who are diagnosed with BCC have a 35% chance of recurrence at the same site within 3 years and a 50% chance of developing another (not recurrent) BCC within 5 years [12].
Notes
No potential conflict of interest relevant to this article was reported.
Appendices
CME Test : Basal Cell Carcinoma
1. What is the most common type of basal cell carcinoma of the head and neck?
Nodular basal cell carcinoma
Superficial basal cell carcinoma
Morphoeic basal cell carcinoma
Cystic basal cell carcinoma
2. Which of the following treatment methods for basal cell carcinoma has the lowest 5-year recurrence rate?
Surgical excision
Radiotherapy
Cryotherapy
Mohs micrographic surgery
3. Which area has the highest rate of recurrence for basal cell carcinoma?
Forehead
Nose
Ear
Hand