Nicolau Syndrome after Intramuscular Injection: 3 Cases
Article information
Abstract
Nicolau syndrome is a rare complication of intramuscular injection consisting of ischemic necrosis of skin, soft tissue, and muscular tissue that arises locoregionally. The characteristic pattern is pain around the injection site, developing into erythema, a livedoid dermatitis patch, and necrosis of the skin, subcutaneous fat, and muscle tissue. Three patients were injected with drugs (diclofenac sodium, ketoprofen, meperidine) for pain relief. Three patients complained of pain, and a skin lesion was observed, after which necrosis developed on their buttocks. Each patient underwent debridement and coverage. The wound healed uneventfully. We report three cases of Nicolau syndrome in the buttocks following diclofenac intramuscular injection.
INTRODUCTION
Nicolau syndrome is a rare complication of intramuscular injection leading to ischemic necrosis of the skin, soft tissue, and muscular tissue that arises locoregionally. Since Nicolau reported the first case of the symptoms as having occurred after intramuscular injection of Bismuth salt for the treatment of syphilis in the early 1920s, cases of Nicolau syndrome have been reported after intramuscular injection of non-steroidal anti-inflammatory drugs, steroids, and other drugs.
The pathogenesis of necrosis is not known completely; it is presumed that ischemic necrosis is induced by direct vascular injury, perivascular inflammation, and vascular constriction. Typical findings are pain at the injection site developing into erythema or hemorrhagic lesion immediately after the injection, with eventual progression to necrosis of the skin or soft tissue, and of the muscle. Among the drugs associated with this syndrome, nonsteroidal anti-inflammatory drugs in particular have rare, severe complications of intramuscular injection leading to necrosis of the skin, subcutaneous tissue, and muscle tissue. The authors report three cases of Nicolau syndrome after diclofenac intramuscular injection.
CASES
Case 1
A 73-year-old man received an intramuscular injection of diclofenac sodium at the orthopedic clinic for lumbar pain control three times a week for 1 month. The patient complained of pain in the upper right buttock after the injection. Three days later, the patient developed pain and redness at the injection site. After one week, a skin lesion was observed and necrosis developed.
At admission, a necrotic ulceration measuring 6×9 cm was found involving the gluteus maximus fascia of the right upper buttock. A pocket 6 cm deep was formed and a severe Pseudomonas aeruginosa infection was identified (Fig. 1). Ticarcillin sodium treatment was started. With four applications of negative pressure dressing therapy, the infection and inflammation were controlled well and granulation began to fill the pocket from the inside (Fig. 2). Two months later, the ulcerative lesion was filled with healthy granulation (Fig. 3) and a split-thickness skin graft was performed. The stitches were completely removed after twelve days. The wound healed well and uneventfully (Fig. 4).

Preoperative view
Necrotic ulceration measuring 6×9 cm was found and a pocket formation 6 cm deep was observed.

After the fourth negative pressure dressing therapy
Granulation begin to fill the pocket from the inside.

After the fourteenth negative pressure dressing therapy
With antibiotics and negative pressure dressing therapy, infection and inflammation was controlled well and the ulcerative lesion was filled with healthy granulation.
Case 2
A 79-year-old female patient was injected with ketoprofen for knee pain relief. After the injection, she experienced severe pain and hardness at the injection site. The wound developed necrotic changes and grew to be 7×5 cm in the subcutaneous layer of her right buttock (Fig. 5). With the concurrent use of antibiotics, the authors performed debridement and direct closure. The wound healed well and the patient was discharged.
Case 3
A 36-year-old man was injected with Demerol (meperidine) every 3 hours during 4 days for operation site pain. After the injections, the patient complained of pain and an erythematous lesion was seen. Two days later, necrotic changes and a purpuric lesion developed. The necrotic wound size was 6×4 cm and the lesion was approximately 13 cm in length (Fig. 6). Histologic findings were superficial and deep perivascular dermatitis with vaculolar change in the epidermis and vasculitis were identified. The authors performed an excision and covered it with a bilateral advancement flap. The wound healed uneventfully.
DISCUSSION
Nicolau syndrome is a rare complication of intramuscular injection leading to ischemic necrosis of the skin, soft tissue, and muscular tissue that arises locoregionally. Several drugs have been reported to cause necrosis, such as local anesthesia [1], antihistamine (promethazine) [1], vitamin B complexes [1], diclofenac sodium [2-4], ketoprofen [2], piroxicam [4], corticosteroids [5], diphtheria, tetanus, pertussis vaccine [6], and meperidine [1].
The pathogenesis of the disease is not known, but there have been several hypotheses. First, it is presumed that the sympathetic nerve is stimulated by pain from the intra-arterial or periarterial injection of drugs, causing vasospasms and leading to ischemia. Second, this is related to the pharmacologic properties of NSAIDS. NSIADS inhibit prostaglandin synthesis by inhibition of cyclooxygenase. Ischemic necrosis occurs after vasospasm are induced by the suppression of prostaglandin by the drug. Third, the intra-arterially injected drug causes embolic occlusion. Nicolau histologically discovered bismuth in peripheral arteries. Fourth, ischemic necrosis progresses from vascular rupture due to perivascular inflammation from a cytotoxic reaction to the drugs. Fifth, lipophilic drugs penetrate the blood vessels in a manner similar to that of fat embolism and induce physical occlusion [1].
Typical findings are pain at the injection site, erythema, or a hemorrhagic lesion immediately after the injection, with eventual progression to necrosis of the skin or soft tissue and of the muscle.
In most cases, the prognosis of Nicolau syndrome is healing with remaining atrophic scars or pigmentation. In rare cases, however, it can cause complications such as hypoesthesia, paraplegia, sphincter deficiency or sepsis.
While various treatments have been attempted for Nicolau syndrome up to the present, none has become standard. In most cases, conservative treatment such as pain control, antibiotics, and dressing may help, depending on the symptoms, and surgical methods, including debridement and skin graft, are required for necrotic areas not showing significant improvement [3]. Besides these methods, improvement has been observed with anticoagulants and vasodilators.
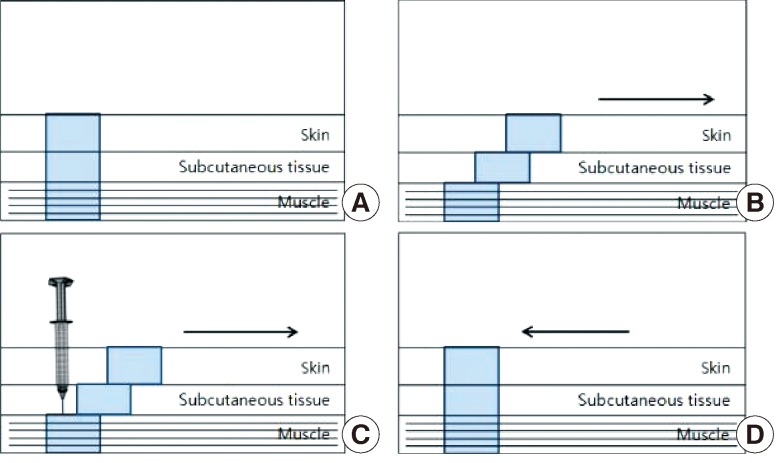
Although the onset of Nicolau syndrome cannot be predicted, to reduce the risk of tissue damage as much as possible, injection is administered to the superolateral region of the gluteal muscle, for which an injection needle is used that is long enough to reach the muscle. It is recommended that the injection be administered using the Z-track method (Fig. 7) [7], and that intramuscular injections not be repeated in the same region. Moreover, if there is an attempt to inhale the syringe and if pain occurs during the injection, immediate discontinuation of the injection is recommended [1].
Notes
This study was presented at the 67th Congress of the Korean Society of Plastic and Reconstructive Surgeons on Nov 19-21, 2009 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.