Early Intervention for Low-Temperature Burns: Comparison between Early and Late Hospital Visit Patients
Article information
Abstract
Background
Various focal heating devices are popular in Korea under the cultural influence of the traditional ondol under-floor method of home heating. These devices can cause severe burn-like injuries resulting from device malfunction or extended with low heat contact. In addition to injuries under these high heat contact, burns can be occurred by low heat exposure with prolonged periods despite the devices are properly functioning. In order to develop strategies to reduce the duration of periods of illness due to low-temperature burns, we analyzed and compared treatment methods and therapeutic periods for this type of injury.
Methods
This retrospective study included 43 patients burned under low heat conditions. Patients were divided into an operative group and a conservative group. The patients in the operative group underwent at least one surgical excision, and were further subdivided into early and late visit groups. The conservative group was treated only with dressings. We compared the treatment periods between the operative group and the conservative group, and also compared the preparation periods and treatment periods between the two operative groups.
Results
The average treatment period was significantly shorter in the operative group (P=0.02). In the early visit operative group, both wound preparation and treatment were briefer than in the late visit group.
Conclusions
We recommend that early proper burn care and early surgical intervention, including appropriate excision, are feasible ways to reduce the treatment period of low-temperature burn patients.
INTRODUCTION
The traditional Korean floor heating system, called ondol, keeps residents comfortable, despite low indoor temperatures, by under-floor heating. Koreans' familiarity with this system has led to their use of focal heating devices, such as electric pads and hot packs, as substitutes for a heated floor. Although these devices maintain a surface temperature of around 50℃, they can often cause severe burns, because people usually use these devices while sleeping, leading to exposure of the skin to low heat for a prolonged period. Song et al. [1] noted 402 of 4,321 patients with burn injuries were contact burns and the causes were ondol (n=48, 11.9%), hot pack (n=45, 11.2%) in Korea. These types of burns are mainly small, superficial lesions; however, some lesions are deeper than second-degree burns and necessitate surgical intervention.
Burns caused by high temperatures are very painful and destructive. Many studies report that early surgical excision of the burn wound with a proper wound closure strategy can shorten illness duration and even reduce mortality in extensively burned patients [2,3,4,5]. In contrast, burns occurring at low temperature seem to be initially mild and not too painful; however, for this reason, the victims are less aware that the burn has occurred. Hence, patients tend to delay seeking specialized burn care. However, early and specialized care is also necessary for low-temperature burns, because these often cause second- or third-degree lesions. Moreover, if the dermal layer is burned at any temperature, the wound becomes worse the greater the depth within the initial 48 hours [6]. Therefore, low-temperature burn injuries should be considered equally as serious as burn injuries caused by contact with a high temperature. In this article, we analyzed low-temperature burn cases and compared therapeutic methods and treatment periods in each case, to determine the requirements for the proper care of low-temperature burns.
METHODS
Of 1,081 patients with burn injuries treated in our clinic from January 2007 to January 2014, 43 patients received burns due to prolonged exposure to low heat. Approval for the study was obtained from the Institutional Review Board on human subjects research and the ethics committee (IRB No. 2014-07-011). The medical records of these 43 patients were reviewed and analyzed retrospectively. The cause, burn depth, wound size and location, and the presence of underlying illnesses were identified, and the delay between burn onset and the first visit to our clinic, and the delay between the first visit and surgical operation were designated as wound preparation periods. We reviewed the treatment methods and periods of treatment in our clinic from the first visit until wound healing. We classified the depth of injury according to the state of the injury when the patients first visited our clinic and the history of wound progression before the first visit from the onset of the burn, because we did not see the initial state of wounds due to the delay in visiting the clinic. At the first dressing, wounds that presented with bullae and a pain sensation without eschar were regarded as second-degree. If there was dried and painless eschar, or a wound was covered with white or yellowish necrotic tissue, we considered the wound to be third-degree.
The patients were divided into two groups: an operative group and a conservative treatment group. The operative group consisted of patients who underwent surgical excision and any subsequent procedure to cover the defects resulting from the excision. The patients in the conservative treatment group were treated only with dressings, without any surgical excision. We recommended surgical intervention to all patients, because depth of the burns were deeper than deep second degree when we saw at first hospital visit. In the conservative group, patients who refused any operation were included although they were recommended surgical treatment. After dividing the patients into the two groups, we compared the therapeutic periods between the two groups. In the operative group, wound healing was regarded as complete on the postoperative day when all stitches were removed, providing that there were no complications such as wound dehiscence or skin necrosis. If complications remained on the day when all stitches were removed, the endpoint of treatment was considered to be the time at which the defects were epithelized and no longer required dressing. In the conservative group, the endpoint of treatment was the same as described above for the operative group with complications.
In addition, we compared the wound preparation periods within the operative group. We defined the preparation period as the time from the first visit until surgical intervention. Since almost all wounds showed inflammatory signs, such as redness around the wound margin, local heat sensation, induration, pus-like discharge, or abscess, we decided to perform surgical intervention after the inflammatory signs had subsided. During the preparation period, the patients were treated with wound dressing procedures at least every other day, and these included individualized options like brief curettage, simple incision and drainage in the case of abscess, and empirical antibiotic therapy. We divided the operative group into an early visit group and a late visit group. The early visit group consisted of the patients who visited our clinic within 15 days of the burn onset, while the patients who visited our clinic 15 days after burn onset were sorted into the late visit group. The comparison of the preparation periods and the treatment periods was performed between the two groups. Also, several factors which could influence on the treatment periods were compared, such as age, diabetes mellitus and albumin level.
Statistical analysis was performed using STATA ver. 12.0 (Stata Corporation, Lakeway, TX, USA). The two-sample Wilcoxon rank-sum (Mann-Whitney) test was used to measure statistically significant differences in treatment periods between the operative and the conservative group, and between the early visit group and the late visit group. In addition, we used the same test to assess the statistical difference between the wound preparation periods. A P-value of less than 0.05 was considered statistically significant.
RESULTS
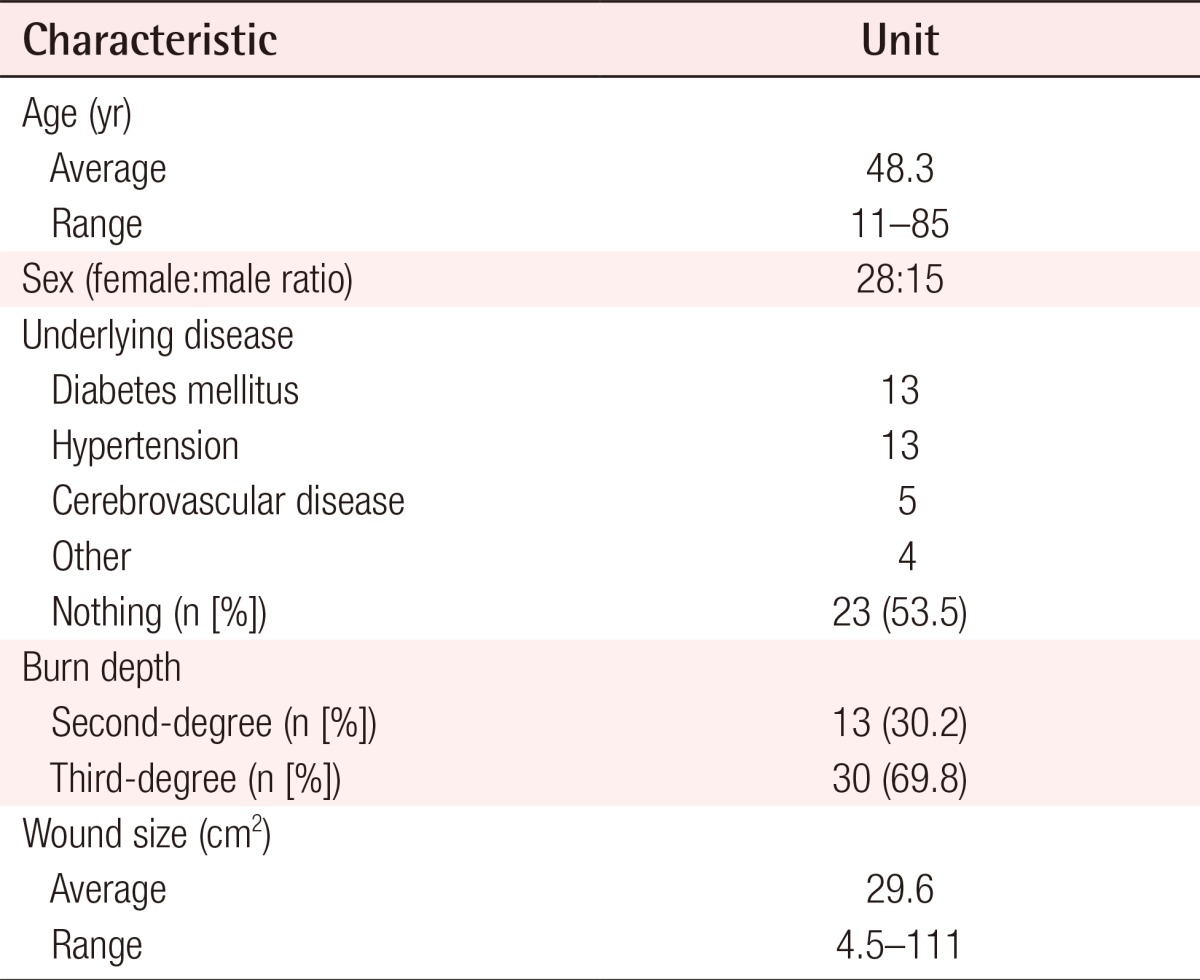
A total of 43 patients were included in this study, consisting of 28 males and 15 females. The average age of the patients was 48.3 years, and patient ages ranged from 11 to 85 years old. There were 23 patients with no underlying disease, and the remainder of the patients suffered from one or more diseases such as diabetes mellitus, hypertension, or cerebrovascular disease (Table 1).
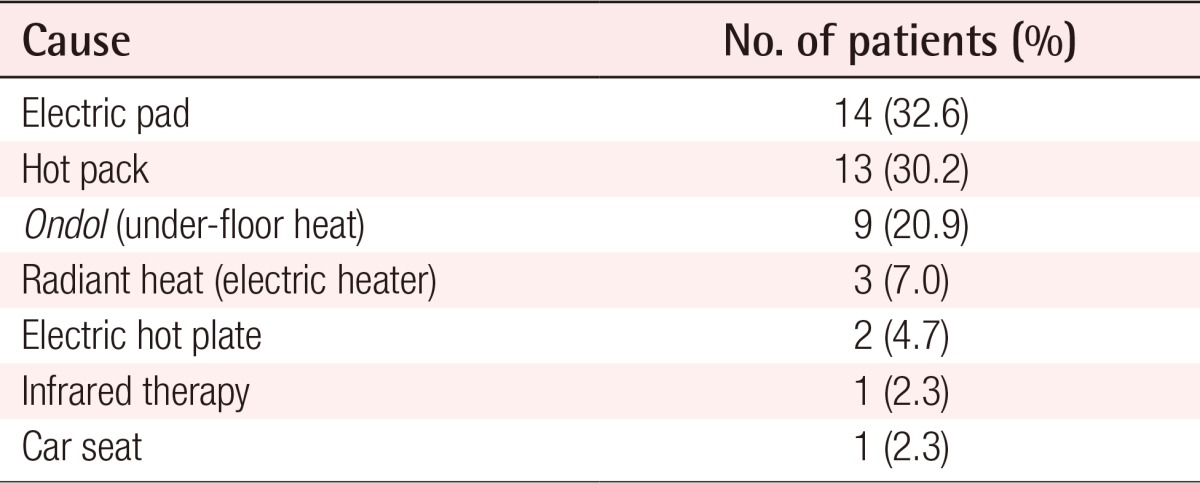
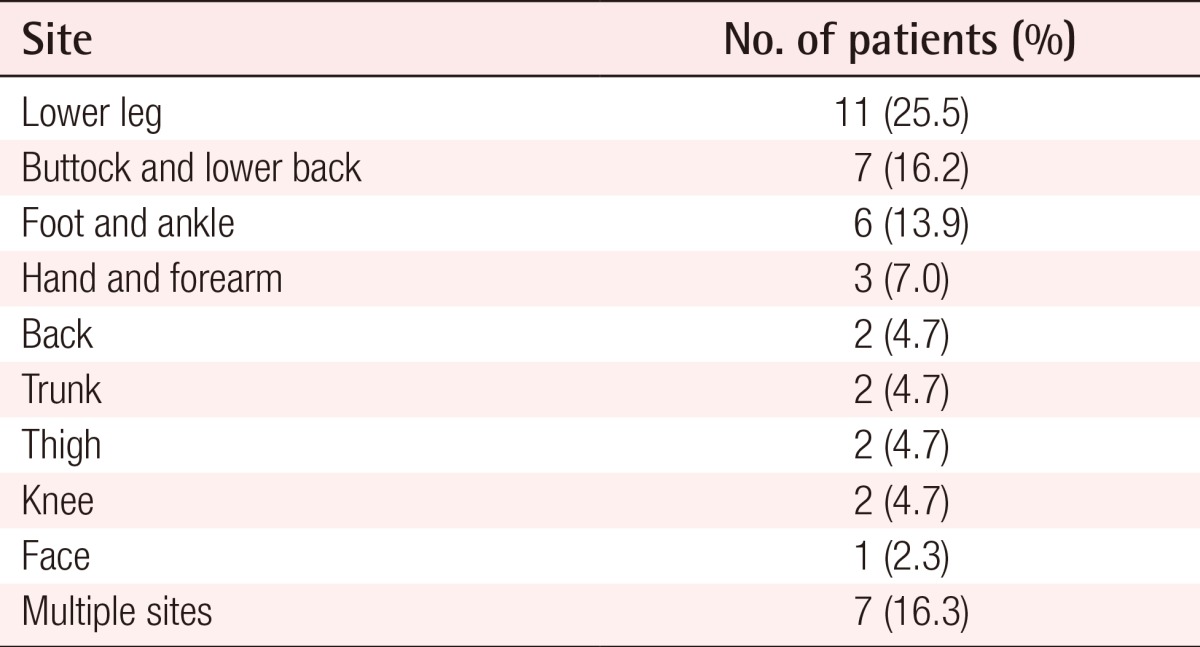
The electric pad was the most common cause of low-temperature burn injury, followed by the hot pack and the ondol floor (Table 2). The majority of burns were third-degree (69.8%), with the remainder being second-degree (30.2%). All second-degree burn patients were treated conservatively. The average burn wound size was 29.6 cm2 and the wound size ranged from 4.5 to 111 cm2 (Table 1). The most frequent site where burns occurred was the lower leg, followed by the buttock and lower back region, foot and ankle, hand and forearm, and other sites (Table 3).
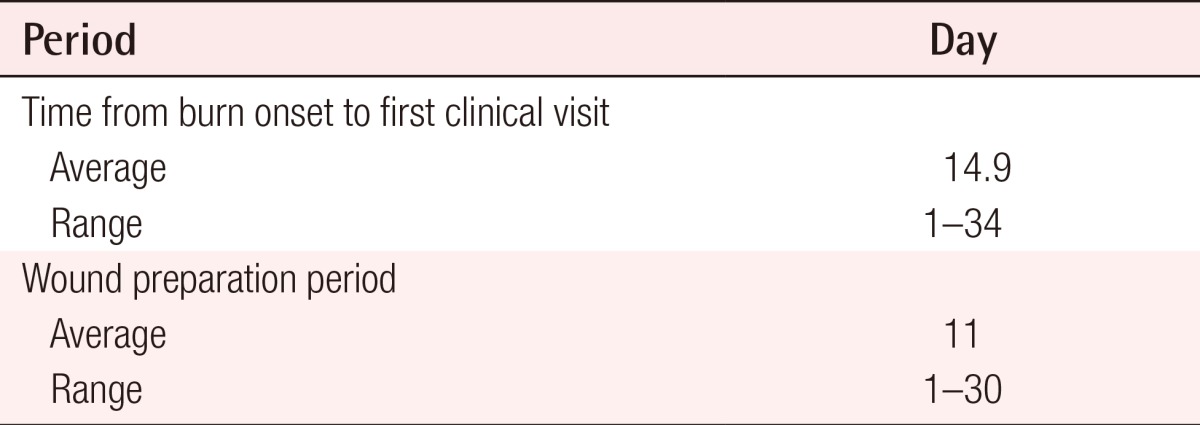
The patients visited our clinic for specialized burn care around 15 days after onset of the burn. Before they were treated in our department, some of them had treated themselves, while others were treated by doctors who did not specialize in burn care. 17 of the patients tried to treat the wound without specialized care for 2 weeks to 1 month; however, the patients reported that the wounds did not improve during that period. A total of 23 patients underwent surgical interventions, such as skin graft, flap coverage, primary closure, and surgical excision. In this operative group, there was an average of 11 days between the first visit and surgical intervention, and the range of this preparation period extended from 1 day to 30 days (Table 4).
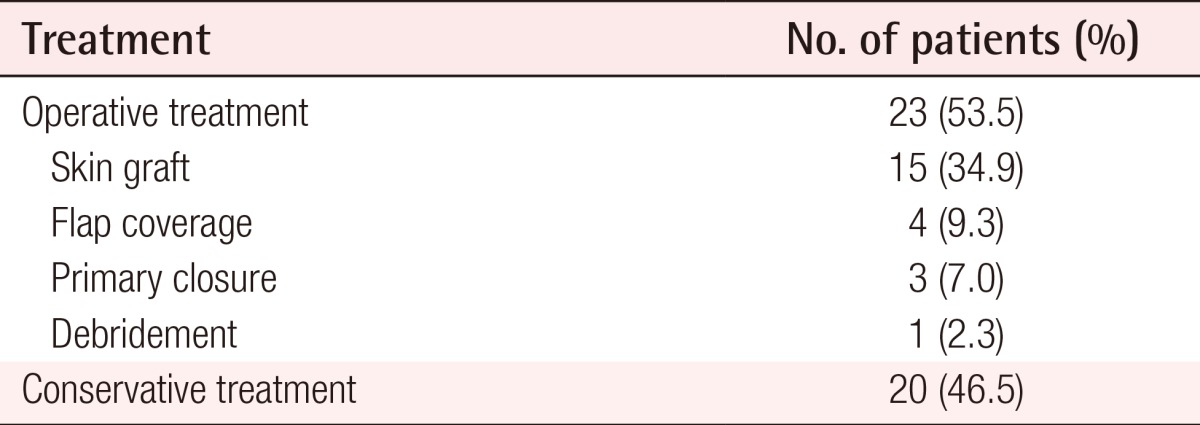
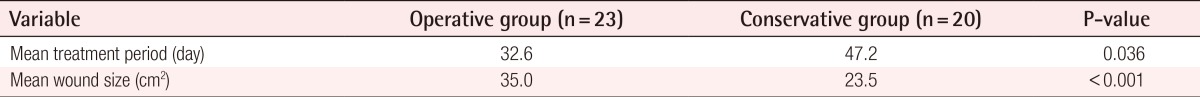
Among the 23 patients who underwent surgical intervention, skin grafts comprised 15 cases, and all grafts were performed as split-thickness skin grafts. Four patients underwent flap coverage; this included 3 advancement flaps, including the V-Y advancement technique, and one perforator-based island flap. There were three cases treated by primary closure after surgical excision, and one patient underwent only surgical excision and dressing. In contrast, there were 20 patients who were treated with dressing only (Table 5). In the operative group, the average treatment period was 32.6 days; in contrast, healing took 47.2 days in the conservative group. This difference was statistically significant (P=0.036), and indicated that a shorter period of treatment was observed in patients who underwent an operation (Table 6).
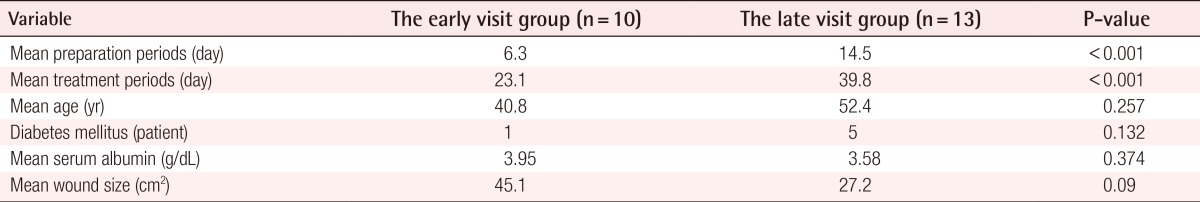
Among the 23 patients in the operative group, 10 patients came to our clinic within 15 days of the occurrence of the burns. The remaining patients visited our clinic between 15 to 34 days after burn onset. Most of the late visit group treated their wounds at local hospitals or at home initially, however the wounds did not improve. As a result, these patients sought our clinic more than 2 weeks later. It took an average of 6.3 days until the inflammatory signs subsided in the early visit group, and 14.5 days in the late visit group. The preparation periods were significantly shorter in the early group (P<0.001). The same result was found in the comparison of treatment periods: in the early group, the patients were treated for an average of 23.1 days; however, treatment took 39.8 days in the late group (P<0.001). No complication was found after operation such as wound dehiscence, skin loss, hematoma, or infection in these two group. There was no significant difference in age, diabetes mellitus, serum albumin and wound size between the early and the late groups (Table 7).
DISCUSSION
Many focal heating devices are popular in Korea, under the cultural influence of the traditional ondol under-floor heating system. Because Koreans mainly use electric pads, hotpacks and ondol floor heating when they sleep, the skin is exposed to heat for a prolonged period. Hence, many people receive burns even though these devices maintain a surface temperature at a relatively low temperature of 50℃ [7]. An individual lying on top of a heated electric pad, ondol, or hot pack all night can unconsciously receive burns that extend underneath the dermis and even to the muscles. In these cases, the burn site is mostly dependent on the position of the body, such as the posterior side of the lower leg, buttock, lower back or heel. The contact area is not limited to a single region, so that burns often occur at multiple sites. The size of the burn also varies according to the cause, with the average wound size in our study being 29.6 cm2 and the largest wound 111 cm2. Individuals that suffer from diabetes mellitus, can get burns more easily, since patients with this illness are desensitized to thermal sensation due to diabetic neuropathies. Mun et al. [8] reported that patients with diabetes mellitus who were burned by exposure to low heat stayed longer in the hospital than those patients without the disease.
Most people who were burned at relatively low temperatures were not aware of their injuries. Some patients even had no concern about the wounds when they found them, because they did not suffer pain at the time of injury. This diminished perception of the seriousness of low-temperature burns means that patients may miss the critical window for proper initial burn care. In this study, it took an average of about two weeks until the patients visited a specialized burn care clinic. In many cases, low-temperature burns presented as deeper than second-degree. It is reported that temperature and duration of contact have synergistic effects on burn injuries. Only a second of exposure to a temperature of 69℃, or an hour at 45℃, can cause cell necrosis [9]. At a constant surface temperature, more heat is accumulated with prolonged exposure time [10]. Because of this, although the devices maintain a low surface temperature, a severe burn injury is still likely to occur.
If burns with eschar, or covered necrotic tissue, occur, these should be removed or debrided early to improve wound healing [2,3,4,5]. The longer proper care is delayed, the longer the treatment periods, and the more expensive the costs, because of the increased risk of complications. In our study, some patients were treated with antibiotics and dressings over two weeks because of inflammation, cellulitis or abscess formation before operation. Most of the late visit group delayed seeking proper care, and needed longer preparation periods. As a result, treatment took longer periods than in the early visit group. As described above, the mean preparation and treatment periods were much longer in the late visit group. In addition, there was a difference between these two groups in postoperative treatment periods. The early visit group required fewer days after the operation for wound healing. We suggest that these results are due to complications, since in most of the patients in the late visit group inflammation accompanied the burn injuries, which hindered the wound healing process after operations. These unnecessarily lengthy treatment periods can be reduced by initial proper treatment and early surgical intervention.
The treatment periods from the first visit to our clinic until the endpoint of treatment were analyzed and compared between the operative group and the conservative group. The treatment periods were significantly shorter in the operative group, as we described above, despite the conservative group consisting of patients with milder burns than those in the operative group: the operative group consisted entirely of third-degree burn patients, whereas the conservative group consisted of second-degree and small third-degree burns. Second-degree burn patients accounted for half of the conservative group. This means that a low-temperature burn is a sufficiently severe problem to cause deep burn injuries underneath the dermal layer that need surgical intervention and specialized care. We treated the operative group with split-thickness skin graft, flap coverage techniques, or primary closure. Some of the late visit group, however, required more than four weeks until wound healing after operation. They had already experienced a period of prolonged illness while the inflammation subsided; however, a subsequent healing period after the surgery was also necessary. We considered that the reason for this prolonged healing was related to the zones of burn injuries and the delayed medical evaluation of the wound. When a patient visited our clinic about two weeks after the onset of burns, the reversible area, called the zone of stasis, appeared grossly normal. If there are no infectious signs or indurations in the surrounding area of a necrotized wound, its color and turgor are similar to normal tissue, and the wound seems to be completely demarcated. In these cases, it is likely that debridement was limited to the grossly necrotized area. However, the blood flow to the zone of stasis may be reduced, due to microthrombi and there remains residual inflammation as a result of initial thermal injury [11], changes that hinder proper wound healing, and often lead to a relapse of inflammation after surgery. In fact, relapsed infection and wound dehiscence were found in patients who were treated over four weeks after the surgery. Hence, we recommend that debridement should be performed to include damaged tissues that look like normal skin, prior to any coverage procedures [12,13].
Unfortunately, we did not undertake any pathological tests to confirm residual inflammation or irreversible changes that might interrupt wound healing in the zone of stasis, and thus could not identify with certainty the reason for delayed healing after surgical excision in the late visit group. We suggest that a larger scale study of low-temperature burns that includes pathological analysis will make a great contribution to establishing the ideal treatment strategy for this condition.
Low-temperature burns appear to be simple and mild burns; however, in fact, they can cause severe illness. Therefore, the public should be educated to seek proper management of these injuries as soon as possible, in accordance with the approach to severe burns. Moreover, early surgical intervention, including a suitable extent of excision, may be a practical way to reduce the periods of illness experienced by patients with low-temperature burns.
Notes
This study was supported by the research fund of Hanyang University (HY-2014).
This article was presented at the 72th Congress of Korean Society of Plastic and Reconstructive Surgeons on November 7-9, 2014 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.