Incorporating a Racket-Handle Skin Bridge and Venous Supercharging to Improve Reliability of the Distally Based Anterolateral Thigh Flap
Article information
Sir,
The distally based anterolateral thigh flap is one anatomical variant of the versatile regional flap commonly employed to reconstruct large knee defects [1]. Venous congestion poses a common concern for such flaps as oedema can potentiate complications such as tip necrosis and eventually scar development. To limit loss of mobility secondary to scarring in the knee, the surgeon should take a preventative approach and optimise venous drainage when utilising anterolateral thigh flaps. We present a case combining two manoeuvres, the racket handle with skin bridge technique [2] and anterograde venous drainage augmentation [3] to maximise venous outflow.
Our 62-year-old patient presented with an open patella fracture sustained in a road traffic accident where initial treatment including wound debridement and cerclage wiring was performed. Concurrent skin loss sized 12 cm by 6 cm over the knee was resurfaced later with an anterolateral thigh flap. During the reconstruction, we located the dominant cutaneous perforator in the distal thigh and traced it back to the descending branch of the lateral femoral circumflex artery. The proximal descending branch was clamped with a micro-clamp before division to check that there was adequate retrograde perfusion. In this case, we noted that the distal segment was still pulsating strongly after clamping, indicating robust arterial flow from collateral supply in the knee [2]. Maximisation of venous drainage is imperative in these flaps to reduce risk of congestion and subsequent complications such as necrosis, scarring and flap loss (Figs. 1,2,3,4,5).

We planned to preserve a skin bridge in the distal flap, the pivot point for rotational transposition, which acted as a channel for venous outflow.

Two cutaneous perforators were identified and shown to be strongly pulsatile even after the descending branch was clamped proximally.

The great saphenous vein was mobilised to the descending lateral circumflex vein so an anastomoses can be formed after flap transposition.

At two year follow-up the defect has been closed with little overlying tension and minimal scarring allowing for acceptable range of movement. Minor scar revision of the dog-ear over the pivot point of the flap had been done.
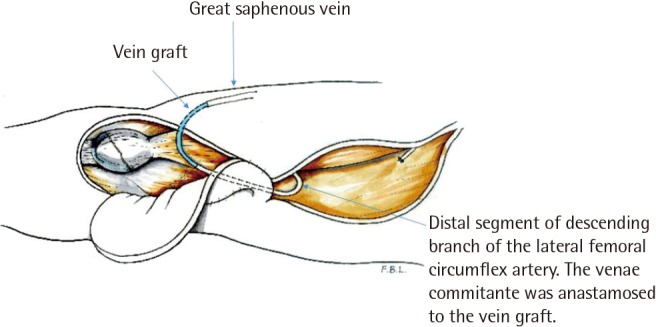
Diagram of the transposed anterolateral thigh flap after anastomosing the main pedicle vein with the great saphenous vein.
Two manoeuvres were employed in this case to improve venous drainage; the first was a racket-shaped design which gently tapered into a short "handle". This was a full-thickness skin bridge at the pivot point where the proximal flap was rotated 180 degrees downward towards the recipient site. The bridge acted to offer cutaneous and subcutaneous continuity and maintained an intact subdermal plexus to serve as additional channel for venous drainage [2]. After the flap was transposed to the knee, a vein graft was utilised to connect the descending femoral circumflex vein to the great saphenous to further augment drainage [3].
The patient experienced no evidence of postoperative flap congestion despite being at higher risk due to his large flap and at two year follow-up, showed good mobility ranging between 0 and 120 degrees flexion in the knee.
Anterolateral thigh flaps are well understood and the anatomy well delineated, offering a large expanse of skin commonly utilised as free flaps. The distally based variant, supplied by retrograde arterial flow, can be used for coverage of knee defects [1]. Robust retrograde flow was observed intraoperatively in our case, likely secondary to medial geniculate contribution. Our concern was with insufficient venous drainage risking flap congestion and subsequent development of marginal flap necrosis [3]. The case illustrates two techniques available to alleviate venous congestion with either the preservation of a dermal and subcutaneous bridge in our racket handle or the anterograde anastomosis of a distal vein to drain the main pedicle vein. Although both techniques have been employed in this case to optimise venous drainage, each strategy is probably sufficient by itself to enhance venous outflow as there will be situations when only one is feasible. A skin bridge is unadvised in obese patients, as the thickness of subcutaneous fat physically restricts the pivoting of the flap, greatly limiting its reach. Conversely, venous anastomosis may be impractical in cases where the great saphenous vein is thrombosed, inflamed, or previously harvested for coronary bypass surgery.
Notes
No potential conflict of interest relevant to this article was reported.