The Oblique Rectus Abdominis Musculocutaneous Flap for Reconstruction after Resection of a Spermatic Cord Liposarcoma
Article information
A 62-year-old Chinese man presented with a painless swelling in the right inguinal region that had been increasing in size for over a year. After ultrasound imaging, a provisional diagnosis of a spermatic cord lipoma was made, and the inguinal mass was excised. The histological examination revealed a well differentiated liposarcoma with involved margins.
The patient was referred to a urologist at our institution for further management. On examination, a right inguinal scar was noted over a 7-cm swelling in the right inguinal region. The right testis was firm, enlarged, and fixed to the surrounding right hemiscrotal skin.
Surgical resection of the right inguinal region and the right hemiscrotum, in combination with right orchidectomy, resulted in a 20×8-cm skin defect and a 5×3-cm anterior abdominal wall defect involving the external oblique aponeurosis, internal oblique muscle, and conjoint tendon, and extending along the inguinal canal (Fig. 1). A contralateral oblique rectus abdominis myocutaneous (ORAM) flap was raised based on the left deep inferior epigastric vessels. The inguinal fascial defect was reconstructed with the size-matched anterior rectus sheath of the ORAM flap by sequential mattress stitching that opposed the edges of the inguinal fascial defect to the rectus sheath of the flap (Fig. 2). The skin and subcutaneous defect were closed with a skin paddle. Excess length at the distal end of the skin paddle was de-epithelised and folded onto itself to obliterate the potential hemiscrotal dead space and create fullness in the scrotum after the orchidectomy (Fig. 3). An inlay prolene mesh was used to reconstitute the defect in the donor site rectus sheath followed by meticulous closure of soft tissue and the skin in layers. The patient had an uncomplicated recovery. A follow-up examination three months later showed that his wounds had recovered well, with good aesthetic results (Fig. 4). Clinical and radiological investigations did not show any recurrence or complications, such as inguinal hernia (Fig. 5).

Surgical resection of the right inguinal region and the right hemiscrotum, together with right orchidectomy, resulted in a 15×7-cm skin defect and a 5×3-cm anterior abdominal wall defect involving the external oblique aponeurosis, internal oblique muscle, and conjoint tendon. The oblique rectus abdominis myocutaneous flap was raised based on the paraumbilical perforators of the rectus abdominis muscle.

The skin and subcutaneous defect were closed with the oblique rectus abdominis myocutaneous) skin paddle and the excess length at the distal end of the skin paddle was de-epithelised and folded onto itself to obliterate the potential hemiscrotal dead space and create fullness in the scrotum after the orchidectomy.
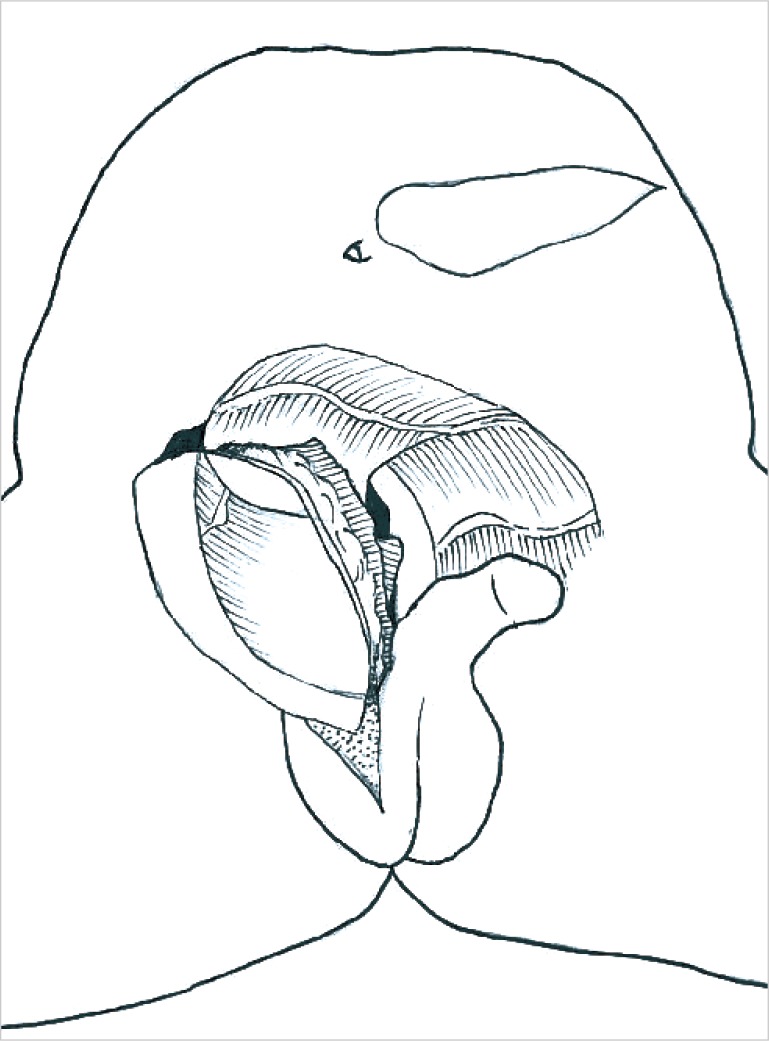
This schematic figure shows how the oblique rectus abdominis myocutaneous flap was tunnelled and folded over, so that the anterior rectus sheath in the flap was used to reconstruct the fascial component of the inguinoscrotal defect.

This figure contains a frontal view three months after the operation showing that the wounds had healed well and that a good aesthetic result was achieved.

This figure contains a lateral view three months after the operation showing that the wounds had healed well and that a good aesthetic result was achieved.
Liposarcoma of the spermatic cord is a rare disorder, and only approximately 100 cases have been reported worldwide [1]. Surgical management usually involves radical excision, and a large composite skin and soft tissue defect is created at or near Hesselbach's triangle, a naturally weakened area of the abdominal wall. A sizable dead space is also created after resection. Defects in the inguinal ligament, lacunar ligament, or conjoint tendon weaken the inferior or posterior border of the inguinal canal, further predisposing the patient to direct inguinal hernias if unrepaired. With these deficiencies in mind, our flap choice was based on the principle of replacing like with like. We required a moderately sized flap with a large reliable skin paddle to fill the dead space and resurface the 20×8-cm skin defect. Primary closure would have resulted in seroma formation in the dead space as well as tightness of the area of the groin crease on hip extension, which can lead to complications involving wound breakdown due to the high tension of the closure. Sufficient fascia should be present on the flap to repair the fascial defect at the inguinal region. Little information on postoperative complications has been published, but we believe that they would include poor wound healing due to excessive wound tension, development of a seroma, infections secondary to a large dead space, flexion contractures of the hip if skin grafts are used, and inguinal hernias due to the loss of the fascial integrity of the inguinal canal.
Careful preoperative assessment of the composite defect and an understanding of the characteristics of each flap allowed us to narrow our flap options to a pedicled anterior-lateral thigh (ALT) flap or a pedicled ORAM flap. The ALT flap is often used to reconstruct defects in the head and neck, perineum, and lower limb, and involves a reliable blood supply that can be raised with a large skin paddle with minimal donor site morbidity. The ORAM flap is a myocutaneous flap based on the periumbilical perforators exiting the rectus abdominis muscle. Cadaveric studies have shown that when the periumbilical perforators were injected with dye, preferential filling was observed in a lateral and superio-lateral-oblique fashion [2]. Skin paddles of up to 43×8 cm in size are reported to have been safely raised [3].
A unique characteristic of the ORAM flap is the differential flap thickness of the skin paddle. It is thick near its origin at the periumbilical perforators, as it includes the full thickness layer of the rectus muscle, and becomes progressively thinner at the distal end. This was ideal for our reconstruction, as we required bulk in the proximal portion of the flap to obliterate the groin and inguinal dead space, while the thin and pliable distal end was used to reconstruct the thinner scrotal and perineal skin. The final results indicated that the soft tissue thickness was a good match to the surrounding skin. The length of the ORAM flap also allowed the tension-free resurfacing of the large longitudinal skin defect from the inguinal ring to the ipsilateral hemiscrotum. The excess skin paddle was de-epithelised and rolled up to fill the remaining area of the scrotal sac. We chose the ORAM flap over the ALT flap for three main reasons. First, a subcutaneous tunnel was created with an oblique projection into the right inguinal scrotal area. It is important to consider the posterior boundary of the subcutaneous tunnel. If this boundary is fixed, it forms a compression point on the vascular pedicle, increasing the risk of flap necrosis. The pliable transversalis fascia and the soft bowel loops form the posterior wall of the subcutaneous tunnel of the ORAM flap, while the relatively thick and inexpansile thigh muscles, femur, and iliac bone form the posterior wall of the tunnel of the pedicled ALT flap. The ALT flap undergoes greater compression in the subcutaneous tunnel than the ORAM flap.
Second, by choosing the pedicled ORAM flap over the pedicled ALT flap, we were able to raise the ORAM flap simultaneously on the contralateral side while the sarcoma was being resected. This resulted in a shorter operative time, less blood loss, and a faster postoperative recovery.
Finally, the arc of rotation of the ORAM flap was preferable to that of the ALT flap, which would have required a 'U-turn' to project the flap into the scrotum.
It is critical to repair the fascial defect at and around the deep and superficial ring of the inguinal canal, as this fascia layer reduces the risk of future inguinal hernias. After measuring the fascial defect over the deep inguinal ring (5×3 cm), we harvested equal dimensions of the left anterior rectus sheath as part of the myocutaneous flap. This anterior rectus sheath was then used after tunneling the flap to close the fascial defect over the deep inguinal ring, replacing like with like. This avoided the use of a synthetic mesh, which would have carried a risk of implant infection as well as being more expensive. Instead of using a mesh to close inguinal fascial defects of this type, it would be more prudent to make use of the fascial component of the flap to reconstruct such defects.
In conclusion, the contralateral pedicled ORAM flap is an attractive reconstructive option after the radical excision of a spermatic cord liposarcoma.
Notes
No potential conflict of interest relevant to this article was reported.