Cross-Leg Flap-Sharing Technique Using an Anterolateral Thigh Perforator Flap
Article information
The need for free tissue transfer to cover defects of the lower legs has been increasing due to the rise in the number of diabetic patients and traumatic injuries, and free tissue transfer has therefore become more popular over the past few decades. It allows for the transfer of well-vascularized tissue to the wound site in a single stage, which leads to early ambulation and improved quality of life. Free tissue transfer has frequently been used to treat defects in the lower extremity associated with trauma, but it has been performed with more reluctance in patients with vascular disease due to the lack of recipient vessels and the poor general condition of such patients, which interferes with prolonged anesthesia. If no acceptable recipient vessel is present in the wounded leg, cross-leg free flaps are available in the extremities. Selecting vessels in the contralateral lateral limb to cover the ipsilateral defect can play an effective role in providing sufficient blood circulation to the transferred tissue [123]. The flap-sharing technique was employed in the reconstruction of two feet wounds due to atherosclerosis, using one flap and a single recipient vessel in the foot to minimize the operation time under general anesthesia.
A 64-year-old man presented to our outpatient clinic with complaints of mummification of the right third and left second toes and bilateral wet gangrene of the foot. This patient had poorly controlled diabetes mellitus and a history of a coronary artery bypass graft seven months previously due to myocardial infarction. He was also a current smoker with a history of 30 pack-years. He had also undergone percutaneous transluminal angioplasty (PTA) to the left common iliac artery and right superficial femoral artery four months previously due to severe atherosclerosis obliterans. The orthopedic surgeon removed the painful areas of gangrene on both feet. Despite long-term wound care, involving negative-pressure wound therapy and the sequential application of split-thickness skin grafts, the foot wounds showed no signs of improvement. The patient was referred to our clinic. Although preoperative computed tomography angiography showed multiple atherosclerotic changes in both lower extremities, the ankle-brachial index was measured using photoplethysmography to be 1.05 in the right ankle and 1.03 in the left ankle (Fig. 1). The pressure ratio of the right dorsalis pedis artery to the brachial artery was 1.01, indicating that it could be safely used as a recipient vessel. Since the wounds were on both feet and one reliable recipient vessel was present, a single anterolateral thigh free flap was planned to cover both wounds in the pattern of a cross-leg free flap.
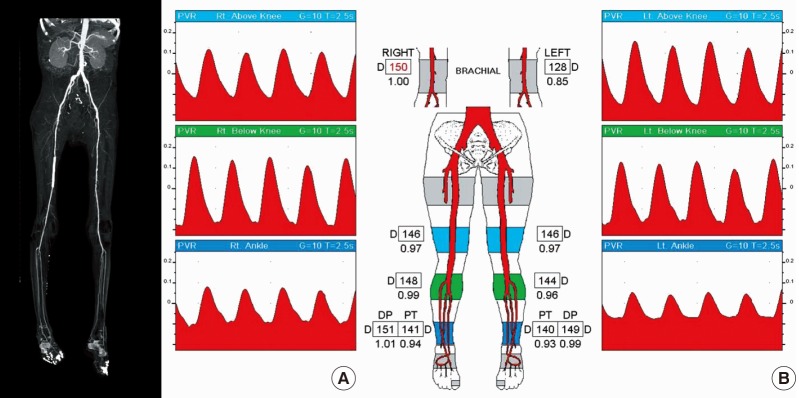
Preoperative computed tomography (CT) scan and photoplethysmography. (A) A CT scan showed atherosclerotic changes in the arteries of the lower leg. The previous angioplasty site can be seen on the left common iliac and right superficial femoral arteries. Stenosis of 50%–75% was found in the left middle superficial femoral artery. (B) The ankle-brachial index was measured to be 1.05 in the right ankle and 1.03 in the left ankle. The pressure ratio of the right dorsalis pedis artery to the brachial artery showed a reading of 1.01, suggesting that it would be viable as a recipient vessel.
First, the devitalized tissue, including the mummified right third and left second toes, was debrided (Fig. 2). An anterolateral thigh perforator flap was then designed to cover the major lateral defects of both feet. The legs were cross-positioned, with the right leg facing upwards, to put the defects close to each other. The right dorsalis pedis artery, chosen as the recipient vessel, was also physically pulsatile and was calibered under a microscope. After inserting the flap into the right wound defect, the arteries were repaired with end-to-side anastomoses, and the veins were repaired with end-to-side anastomoses between the recipient vessel and the vessels of the flap. The remaining portion of the flap was then inserted into the left wound defect (Fig. 3). The two legs were fixed in a crossed position with plaster casts below the knee joints. The donor site was closed primarily. After five weeks of neovascularization, a division was made under local anesthesia. The patient was followed for six months postoperatively (Fig. 4). No complications occurred in the recipient and donor sites during the postoperative period. Several days after the division procedure, the patient complained of aggravated claudication in both lower legs. Angiography was performed in both legs, but no additional vascular complications, such as embolization or restenosis, were found. We observed copious collateral vessels in the distant detached flap on the left foot (Fig. 5)

Previous amputation had been performed on the third, fourth, and fifth left toes and the first, fourth, and fifth right toes. The wound had not improved, so a split-thickness skin graft was performed, but the graft was lost.

After the insertion of the flap into the right wound defect, end-to-side anastomoses were performed between the dorsalis pedis vessels and the vessels of the flap. The remaining portion of the flap was then inserted into the left wound defect.

The patient was followed up for six months postoperatively. No complications occurred in the recipient and donor sites during the postoperative period.
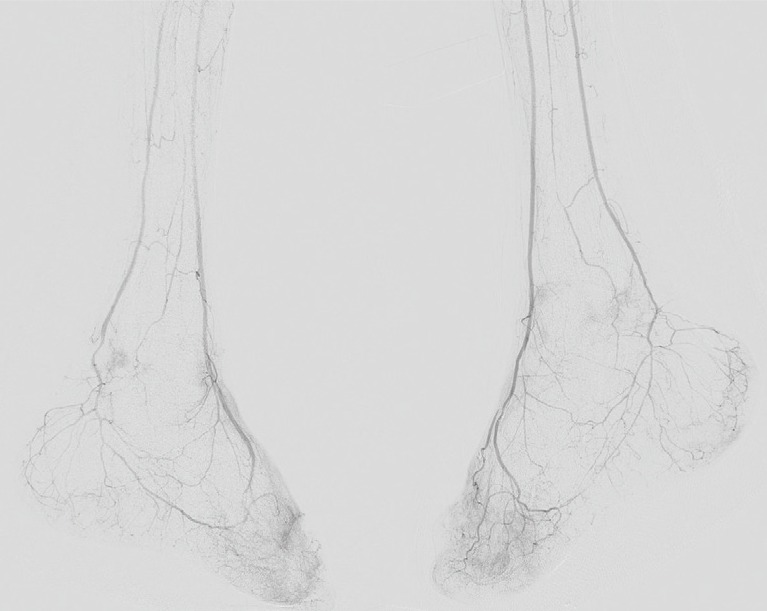
Postoperative angiography was performed one week after division. We observed abundant collateral vessels in the distant detached flap on the left foot.
Free tissue transfer by vascular anastomosis has been performed frequently in a wide variety of wound cases [4]. Cross-leg free flaps and bridging flaps are also techniques for overcoming the lack of recipient vessels adequate for anastomosis in ipsilateral lower extremity defects [3]. To the best of our knowledge, covering defects on both sides via the use of a flap-sharing technique involving crossing the legs and using an anterolateral thigh perforator flap has not been previously reported in the literature. Free flaps are a promising solution, but atherosclerosis is a major risk factor associated with flap failure due to the lack of adequate vessels in the recipient and donor flap areas. Recent studies have shown that small perforators are often spared from atherosclerosis and may be used in these vessels for free tissue transfer [5]. Numerous studies on the combination of vascular bypass surgery and free tissue reconstruction of the lower leg have been published [12]. Since the introduction of endovascular therapy, which is less invasive than conventional bypass surgery, many institutions now propose endovascular treatment prior to free flap reconstruction. In this case, the patient had undergone PTA seven months before the surgery. The procedure would improve the vascular measurement index and vibe on the satisfactory results of the flap. In additional to angiography after the division operation, the distant detached flap was viable due to neovascularization of the surrounding tissue, a phenomenon that has been described in the theory of flap survival in the cross-leg flap technique. Previous reports have shown that the optimal division period for this type of flap is between four and seven weeks after the transfer. However, the time required for the flap to become revascularized from the wound bed is highly variable, depending on the vascularity of the recipient area. The main advantage of this procedure was minimizing the operation time under general anesthesia in a patient with a poor cardiac condition. Using two free flaps simultaneously would have required two donor sites and a longer period of general anesthesia, while using two free flaps sequentially would have required general anesthesia to be performed twice. Although these decisions must always depend on the individual case, prolonged surgery and multiple operations under general anesthesia should generally be avoided in patients with severe atherosclerosis due to associations with higher morbidity and mortality [5].
Notes
This article was presented as an E-presentation at Plastic and Reconstructive Surgery (PRS) Korea 2015 on November 13–5, 2015 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.