Incidental Finding of Mucosa-Associated Lymphoid Tissue Lymphoma during Lower Blepharoplasty
Article information
Recently, the public has developed a growing interest in aesthetic surgery. Middle-aged individuals in Northeastern Asia have have shown particular interest in undergoing blepharoplasty to reduce bulging eyelid fat. However, those who present for aesthetic surgery usually have not considered the possibility of an eyelid tumor, and thus, have not taken time to undergo evaluation for this possibility. Here, the authors describe a case of mucosaassociated lymphoid tissue (MALT) lymphoma that was diagnosed by a thorough physical examination in a man requesting lower blepharoplasty.
A 58-year-old man visited out aesthetic center to alleviate bulging of both lower eyelids, which had begun approximately 5 years previously. The patient had no underlying disease at presentation, and chest X-ray and electrocardiography findings were normal.
Physical examination confirmed bulging of both lower eyelids to a similar extent, and the unidentified tumor was palpated on the left side (Fig. 1). A biopsy was recommended for evaluation purposes, but the patient requested cosmetic surgery only, and thus, we began lower blepharoplasty after informing the patient that a biopsy might be needed during surgery and that if so, additional treatment might be required.

Preoperative photograph: lower eyelid fat bulging was observed bilaterally and an unidentified tumor was tangible on the left side.
Initially, we elevated a musculocutaneous flap by subciliary incision, and then began dissection to the extent of the inferior orbital rim. After exposing the preseptal space, an incision was performed on the orbital septum to expose the orbital fat for removal and transposition. However, we encountered a pinkish, hard, highly vascularized mass-like lesion between the orbital septum and orbital fat, which is not normally found during lower blepharoplasty. After resecting the 1.8 cm×1.5 cm×1.2 cm mass, lower blepharoplasty was performed in the usual manner (Fig. 2).

Intraoperative specimen: a pinkish, 1.8 cm×1.5 cm×1.2 cm mass was found between the orbital fat and orbital septum.
The pathologic examination result indicated MALT lymphoma with an immunoprofile of CD20 (+), bcl-2 (+), CD3 (–), CD10 (–), CD38 (–), and CD138 (–) (Fig. 3). The patient was sent to another hospital for a systematic workup, and subsequent orbital computed tomography (CT) and positron emission tomography (PET)-CT indicated a possibility of residual lymphoma localized in the extraocular area (Fig. 4). As a result, he was treated using involved-field radiation therapy at the origin of the lymphoma at 2 Gy for 20 days based on a 1AE Ann Arbor staging.
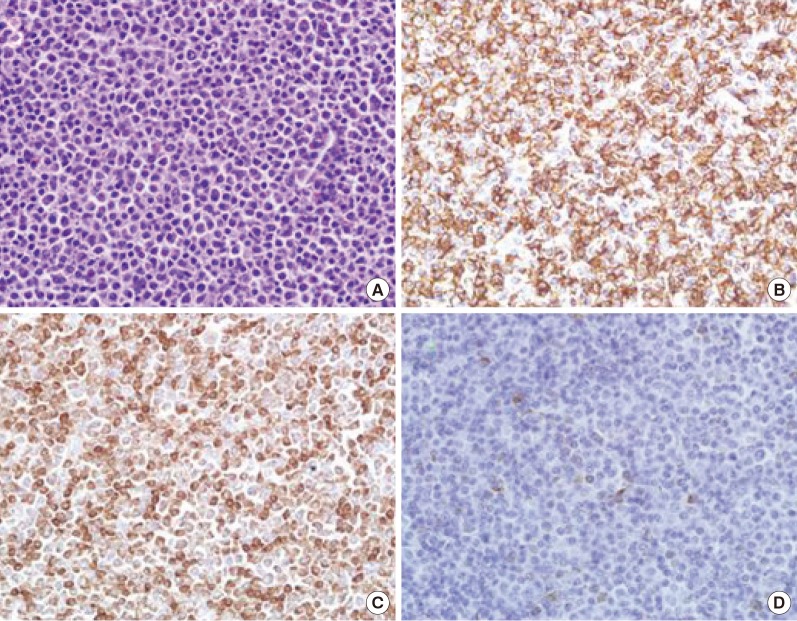
Histopathologic and immunohistochemistry findings: (A) plasmacytoid lymphocyte proliferation (H&E, ×400). (B) CD20 (+). (C) bcl-2 (+). (D) CD38 (–) (all, ×400).
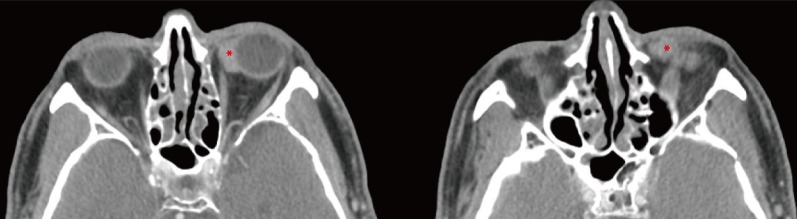
Postoperative orbital computed tomography indicated a possibility of residual lymphoma localized in the extraocular area, on the medial side of the orbit (asterisk).
Orbital CT and PET-CT at 6 months postoperatively revealed no evidence of lymphoma and a good cosmetic outcome was achieved at 6 months after surgery (Fig. 5). The patient was very satisfied with the discovery of the mass at an early stage and the sufficient biopsy.
Primary orbital lymphoma is a rare disease that accounts for 1%–2% of non-Hodgkin lymphoma (NHL) cases. On the other hand, it accounts for 6%–8% of orbital tumors and is the most common malignant tumor found in the adult orbit [12]. Primary orbital lymphoma is usually found in the fifth to seventh decades of life and is more common in women [2]. Since lower fat bulging due to aging usually occurs from the fifth decade of life, patients may be unaware of the presence of a mass. Furthermore, lymphoma usually grows slowly and painlessly (as in our case), which makes detection by the patient even more difficult.
To determine a treatment strategy for orbital lymphoma, clinical staging is crucial, and histopathologic examination is the most important component of staging. In orbital lymphoma, the role of surgery is to collect as much tissue as possible to enable a precise histopathologic examination. In the diagnosis of lymphoma histopathologically, the minimal volume of tissue needed may vary depending on the lymphoma grade. For example, while only a small specimen is needed to identify high-grade lymphoma, a relatively large specimen is needed for differential diagnosis of MALT lymphoma from other conditions (e.g., inflammation) [3]. Therefore, frozen biopsy during surgery is a good way to determine the approximate nature and the free margin of the tumor, if possible.
A cure is dependent on the clinical stage, and the NHL 1AE stage found in our patient can be cured most effectively with radiotherapy [4]. According to one report, simple radiotherapy can enhance the 5-year overall survival rate to 91%–100% for NHL stage 1, which demonstrates that early diagnosis has a major effect on prognosis [4].
Primary orbital lymphoma has been reported on numerous occasions, but the majority of reported cases involve presentation due to a tangible eyelid mass. On the other hand, presentation with a request for lower blepharoplasty because of bilateral lower eyelid bulging and encountering a mass during lower blepharoplasty are extremely rare.
In Northeast Asian countries, people now show great interest in blepharoplasty due to appearance concerns and an aging population. People tend to have thicker, bulging skin in this region. This has resulted in a massive increase in the number of clinics specializing in cosmetic surgery, including blepharoplasty. Given this reality, it is important not to overlook the possibility of a mass resembling fat build-up during blepharoplasty and to take a biopsy sample to check for disease when there is any suspicion. Generally, this advice with regard to checking a described cosmetic problem by meticulous pre-surgical physical and histopathologic examination should be extended to all types of cosmetic surgery.
Notes
No potential conflict of interest relevant to this article was reported.
This article was presented as an E-presentation at the 73rd Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 13–15, 2015 in Seoul, Korea.
