Analysis of Bone Fixation Methods in Digital Replantation
Article information
Abstract
Background
Adequate fixation of replanted digits is essential not only for short-term healing but for long-term function. Various bony fixation methods using Kirschner (K-) and intraosseous wire are available in replantation. We examined clinical and radiographic outcomes of fixation methods on bone union after digital replantation.
Methods
A single institutional retrospective review identified 992 patients who had undergone 1,247 successful replantations between July 2009 and September 2015. Exclusion criteria included amputations of the distal phalanx, comminuted fractures, and intra-articular fractures. Patients were classified according to 5 categories of fixation methods: single K-wire, double longitudinal K-wires, cross K-wires, wire with, and wire without K-wire support. Bone union was evaluated by 5-month postoperative X-ray and fixation outcomes were compared across the 5 groups.
Results
The exclusion criteria were applied, and 88 patients with 103 replanted digits remained for analysis. Single K-wire fixation was used in 40 digits, double longitudinal K-wires in 30, and cross fixation in 14. Wire with and without K-wire support was required in 15 and 4 digits. Nonunion was observed in 32 digits (31.1%), of which 13 required additional operations such as bone graft or corrective osteotomy. The highest percent of nonunion was observed after cross fixation (35.7%) and the lowest after wire alone (25.0%).
Conclusions
In this study, contrary to general knowledge, we found that single K-wire fixation was not associated with poorer outcomes. Successful bone union outcomes may be achieved by careful selection of bone fixation methods. This study provides useful information for planning bone fixation in digital replantation.
INTRODUCTION
Since Komatsu and Tamai [1] reported the successful replantation of a completely amputated digit in 1968, microsurgical techniques and related knowledge have rapidly advanced, and some centers have achieved success rates approaching 90% [2345]. Many authors now emphasize the functional recovery of the restored part, rather than its mere survival, as a significant index of success, and insist on the integrity of bone and soft tissue and long-term results of motion as the better criteria for evaluating outcomes [467].
The foundation of successful functional results is adequate bone reduction and stability, which can permit early motion and future union [7]. Regrettably, problems associated with bone union have occurred at a rate as high as 30% to 40% in some reviews [8].
Bone fixation methods for replantation should be applied in a way that is relatively simple, rapid, and consistent, such that they require minimal injury to bone and soft tissue [910]. Of the many bone fixation methods, single longitudinal K-wire fixation is the best method in terms of rapidity and application, but many hand surgeons do not consider the method suitable for replantation.
Since there are limited comparative replantation studies on the long-term outcomes of bone fixation methods, we have conducted a retrospective study of the digits that were successfully replanted at our center, and analyzed the relationship between skeletal fixation and bone complications. The radiological and clinical results of bone fixation methods involving Kirschner and intraosseous wires and final bone consequences regarding the frequency and percentage of nonunion and reoperation for bone correction were investigated. We have compared the results regarding bone complications between single K-wire fixation and other methods in digital replantation.
METHODS
A single institutional study was conducted retrospectively for patients who successfully underwent digital replantation operations (n=1,247) from July 2009 to September 2015. A retrospective analysis of the medical records of 992 patients was conducted, and demographic information regarding patient age, gender, specific injured body part, fracture type, and operation records was collected.
We have retrospectively selected the amputations with middle and proximal phalanx in an attempt to confine analysis to a relatively homogenous group, and to reduce variability resulting from differing injury levels or severity. Injuries with intra-articular fracture and bone defect—the largest group of patients, accounting for almost 80% of the replanted digits—were excluded from the study. We conducted a study of patients with at least 5 months follow-up with adequate lateral radiographic films.
Following replantation without a bone shortening procedure, the patients wore short arm splints for 2 weeks. After removing the splint, the patients were allowed free finger movement. Before postoperative 3 weeks, physical therapy was initiated. We measured the anterior, posterior, and lateral views of X-rays for bone union and angular deformity, as explained by Coonrad and Pohlman [11], and evaluated initial films performed within postoperative 7 days of replantation and the second X-rays before the beginning of physical therapy. X-rays were performed every 4 weeks for evaluation of union. In all patients, bone union was confirmed by radiographic study (visible fracture gap and sclerosis) and physical examination (pain and instability) at 5 months after the operation.
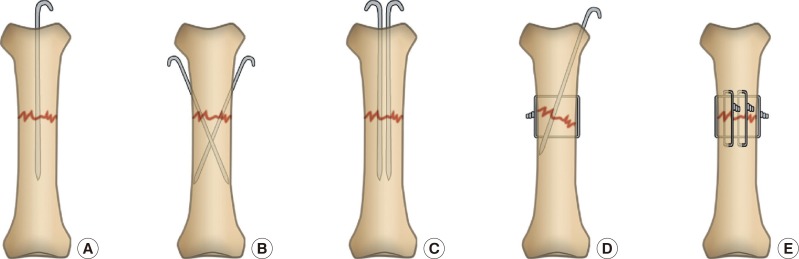
Patients were grouped according to 5 general fixation methods. The final results of bone fixation were compared for single K-wire, cross K-wires, double longitudinal K-wires, and intraosseous wires supported with and without K-wires (Fig. 1). Clinical results, including nonunion, angulation, and additional surgery such as corrective osteotomy or bone graft, were compared.
Techniques of bony fixation
(A) Single K-wire. (B) Cross K-wires. (C) Double longitudinal K-wires. (D) Intraosseous wire with K-wire support. (E) Intraosseous wire.
IBM SPSS ver. 22.0 for Windows (IBM Co., Armonk, NY, USA) was used for statistical analyses of the data, and P-values were determined using the logistic regression analysis, the chi-squared test and the Kruskal-Wallis test to demonstrate outcome differences across the groups. P-values under 0.05 were considered statistically significant. For comparing the complications followed by single K-wire fixation method and other methods, odds ratios were calculated, and 95% confidence intervals were applied where appropriate.
RESULTS
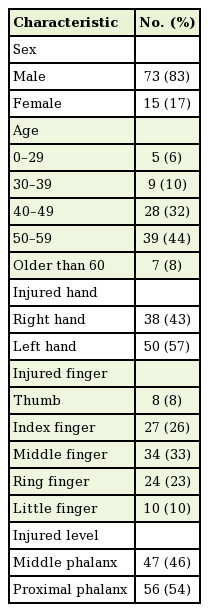
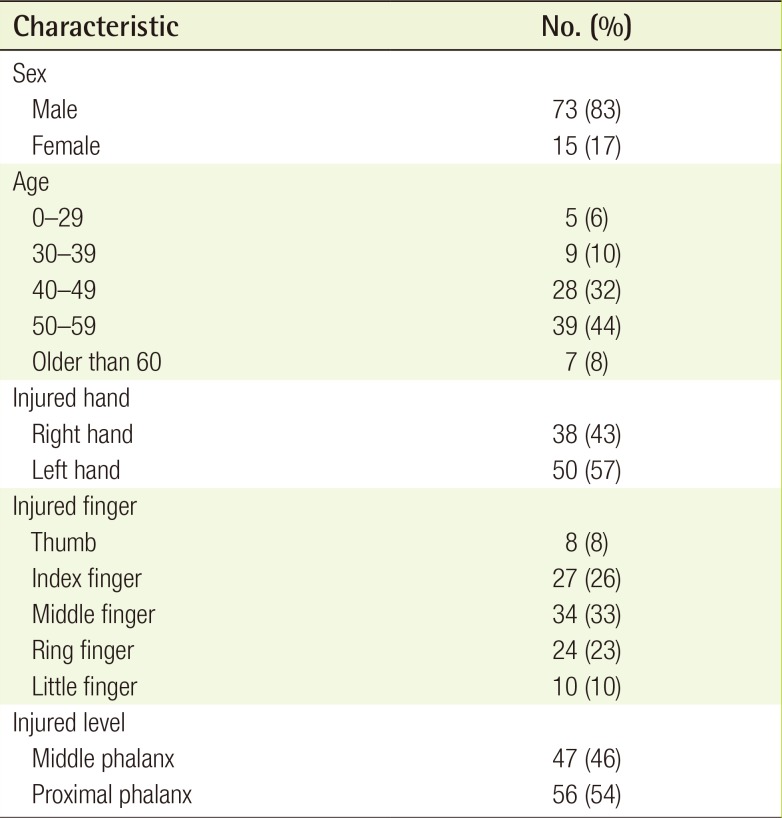
Of the 992 patients identified in the review, inclusion criteria were applicable for 88 patients (103 replanted digits). The mean age was 47 years (range, 2–77 years old). The population was composed predominantly of males, and 54% of digits had proximal phalanx level injuries (Table 1). Single K-wire fixation was used in 40 digits, double longitudinal K-wires in 30 digits, and cross K-wire fixation in 14 digits. Intraosseous wire with K-wire and intraosseous wire without K-wire were required in 15 and 4 digits.
Nonunion
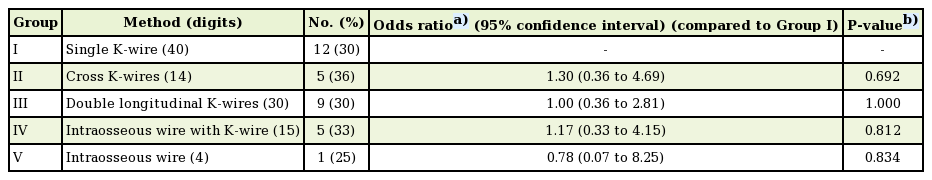
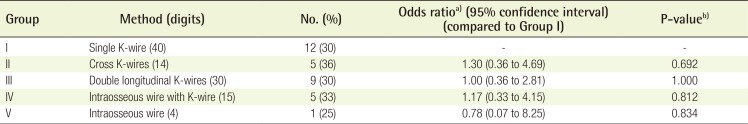
Nonunion for each method is shown in Table 2. Nonunion was observed in 32 digits (31%). The highest rate of nonunion was observed after cross fixation (36%) and the lowest after wire alone (25%). No statistically significant difference was observed among the 5 groups (chi-squared test, P=0.991), and statistics between single K-wire fixation and the other 4 methods were insignificant (chi-squared test, P>0.05).
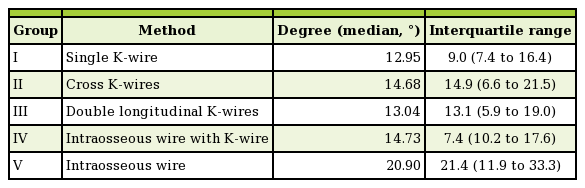
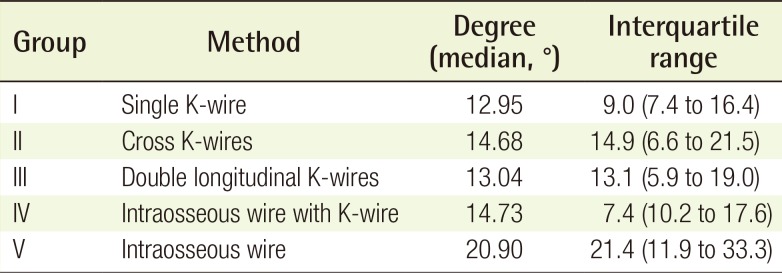
Angulation
The results comparing the 5 methods are shown in Table 3. The duration of fixation was similar in all groups (6.2 weeks), and the mean degree of angulation in all digits was 13.8°. The largest degree of angulation was observed in intraosseous wire alone (20.9°) and the smallest after single K-wire fixation (12.9°). Neither posteroanterior (PA) nor the lateral plane showed statistical difference in all groups (Kruskal-Wallis test, P=0.388).
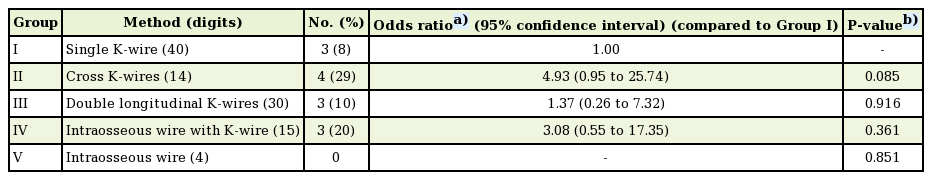
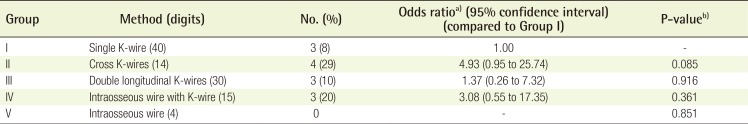
Secondary operation
Thirteen patients underwent a secondary operation due to nonunion, angular deformity, or clinical symptoms. There was no secondary operation after wire alone, and the greatest number of secondary operations after cross K-wires fixation (29%). In the chi-squared test, there were no significant differences in the secondary operation rate depending on the fixation methods (P=0.556) and statistics between single K-wire fixation and the other 4 methods were not significant (chi-squared test, P>0.05) (Table 4).
DISCUSSION
A variety of methods are available for bone fixation. The type of phalangeal fixation in digital replantation has an influence on the operation duration, possibility of early movement, and functional recovery of replanted fingers [1213141516]. The simplest fixation is a longitudinally placed single K-wire. While easily performed, conventional thinking suggests that a single K-wire has some disadvantages: a single K-wire does not provide rigid fixation, does not control against rotation and, almost by necessity, must go through the joint. However, in our study, single K-wire fixation was not associated with poorer outcome in terms of bone complications. Single K-wire is best utilized in digital replants and revascularizations where other fixation methods may not be technically feasible (Fig. 2).

Single K-wire fixation
(A) Little finger amputation in a 52-year-old man. (B) Radiograph shows proximal phalanx amputation. (C) Immediately postoperatively, after digital replantation. (D) Radiograph shows secure fixation with a single K-wire technique. (E) Five-month postoperative radiography with posteroanterior view shows bone union. (F) Five-month postoperative radiography with lateral view shows minimal angulation.
Few authors have reported comparative data with regard to the methods of fixation ordinarily applied with digital replants. In the study of Tamai [3], there were 38 cases of bone and joint complications as high as 16.7%. However, he did not mention the methods of skeletal fixation. Hoffmann and Buck-Gramcko [8] weighed intraosseous wire and K-wire fixation in 68 patients with 90 replanted fingers, and concluded that the former was better in terms of fracture fixation and early hand therapy. Whitney et al. [17] studied 75 replanted digits including the middle and proximal phalanx using 6 methods of bone fixation. Overall, the percentage of complications associated with bone fixation was 50%, the nonunion rate was 16%, and angular deformity occurred in 28%. The reported nonunion rate after replantation varied from 3% to 19% in different series [35817]. As a result of our experience, the nonunion rate was about 31%, which was higher than previous studies. We believe that this is a result of our inclusion of the clinical symptoms as well as radiologic findings in our determination criteria for nonunion.
Few studies quantifying the angulation in long-term bony results have been reported. Because bone stability establishes a basis for allowing the patients' early motion and enhanced long-term results, we attempted to perform a quantitative comparison of ordinary bone fixation methods used in our replantation institution. To avoid confusion by variability and to offer a homogenous population in the method of fixation used, the statistical target was limited to specific levels and similar types of injuries. Amputation procedures performed at proximal and middle phalanx levels, the majority in this study, are the most ordinary area for bony problems in digital replantation, especially with respect to gliding structures and functional outcomes [3518].
Previous authors have suggested that skeletal shortening should be considered in all replantations, which can enable more secure bone fixation and lessen the need for vessel and nerve grafting [19]. Nunley et al. [5] emphasized the necessity of primary bone shortening procedures during replantation of digital amputations, followed by the procedure of K-wire fixation longitudinally in almost all cases. However, in light of our experience, no bone shortening remains the better indication. Primary bone formation occurs under rigid fixation in areas in which bone is held tightly in contact, called “contact healing.” Because there are no gaps in contact healing, Haversian remodeling of the fracture site begins immediately. This Haversian remodeling at the fracture site allows contact healing and results in union and reconstruction of the fracture ends simultaneously [20]. Although more studies are needed, we assume that the larger bone contact area with fitted fracture margin would have an influence on more effective bone union.
Van Oosterom et al. [21] reported that the incidence and cause of surgically corrected phalanx fractures resulted in nonunion. Reported causes for nonunion of phalangeal fractures include high-energy, injury-induced open fracture and bone loss, impairment of blood circulation, infection, skin defect, and damage to soft tissues [2223]. Soft tissue damage disturbs circulation to the fractured fragment and increases the incidence of infection and nonunion. We presume that fixation methods that require more handling during replantation than the single K-wire fixation method generate more soft tissue injury, which can be associated with poorer blood circulation to the bone.
This study has some limitations. In this retrospective study design, a selection bias may have been introduced between patients with worse outcomes and those with better outcomes, who were willing to undergo more diligent or more frequent follow-up. In addition, caution should be exercised in extrapolating this study to the general population of replantation cases. Although the frequency of use of each method reflects our experience with the overall population, the data represents less than 10% of patients referred for replantation. We controlled carefully for the level and severity of injuries; thus these results may not apply to other types of intra-articular injuries or cases of severe comminution. However, we observed no significant difference among bone fixation methods in terms of bone complications, and we suspect that reconstruction of soft tissue and tendons as well as bone fixation resulted in increased stability and rigidity in replanted digits.
As reported by Nunley et al. [5], there are many methods for bone fixation that can provide an adequate fixation. Most surgeons depend on their experience and choose specific methods based on their own subjective results, such that there are few studies about quantitative outcomes concerning bone fixation using more than one fixation method. This study suggests that bone problems following replantation are more common than previously reported, and provides useful information for planning bone fixation in digital replantation.
Notes
This article was presented as a free paper at the 6th Research and Reconstructive Forum on April 7, 2016 in Daegu, Korea.
No potential conflict of interest relevant to this article was reported.