The Role of Negative-Pressure Wound Therapy in Latissimus Dorsi Flap Donor Site Seroma Prevention: A Cohort Study
Article information
Abstract
Background
Donor site seroma is the most common complication after latissimus dorsi (LD) flap harvest. This study aimed to evaluate the efficacy of negative-pressure wound therapy (NPWT) in preventing donor site seroma formation after the harvest of an LD flap for breast reconstruction.
Methods
In this prospective matched-pair study, 40 patients in whom an LD flap was harvested for breast reconstruction were enrolled. NPWT was used in 20 patients, and in a control group composed of another 20 patients, the conventional donor site dressing technique was used. Information was collected regarding postoperative complications, the incidence of seroma, total drainage volume, the number of percutaneous seroma aspirations, and the volume aspirated.
Results
In the NPWT group, the incidence of seroma formation after drain removal was significantly lower than in the control group (15% vs. 70%; odds ratio=0.07; relative risk, 0.24). Both the mean percutaneous aspirated volume (P=0.004) and the number of percutaneous aspirations (P=0.001) were also significantly lower in the NPWT group. There were no significant differences in the total drainage volume or the duration of wound drainage between the NPWT dressing group and the control group (P>0.05).
Conclusions
This study showed that NPWT is a promising tool for reducing the incidence of seroma formation after removing the drain at the donor site after LD flap harvesting. It is a simple and safe technique.
INTRODUCTION
Latissimus dorsi (LD) musculocutaneous flaps are commonly used in reconstructive surgery, particularly in breast reconstruction. Donor site seroma is the most common complication following this procedure, with an incidence varying from 30% to 83% [1-4]. Seroma can be caused by many contributing factors, including shear between subcutaneous tissue and the underlying muscle, dead space, and leakage from lymphatic and vascular channels [5]. Although most patients are asymptomatic, sequelae such as discomfort and infection can be anticipated. Treatments for this problem and preventive techniques have been reported. These methods include avoiding electrocauterization, the quilting of skin flaps and/or the use of fibrin sealant, endoscopic harvest, long-term drainage, pressure dressings, repeated aspiration, sclerotherapy, and steroid injections [5-10]. Quilting of the donor site is the most commonly used technique. However, it is time-consuming and in some patients, exacerbated postoperative pain and restricted shoulder movement have been reported.
The use of negative-pressure wound therapy (NPWT) to stabilize a skin graft by immobilizing the graft, limiting shear stresses, and eliminating fluid collection was described by Schneider et al. [11] and Blackburn et al. [12] in 1998. NPWT addresses factors similar to the mechanisms that cause seroma after LD flap harvest. The aim of this study was to evaluate the efficacy of NPWT as an alternative technique for preventing seroma formation at LD flap donor sites.
METHODS
Patients and methods
The study was approved by the ethics committee of the Faculty of Medicine at King Chulalongkorn Memorial Hospital (IRB No. 030/55). Forty patients, ranging in age from 29 to 55 years, who underwent breast reconstruction using an LD flap between January 2009 and December 2012 at King Chulalongkorn Memorial Hospital in Thailand were enrolled in this matched-pair cohort study. All reconstructive procedures were performed by the same group of surgeons. Patients were divided into an experimental group and a control group. Patients who were operated on by the same surgeon were grouped into pairs and then randomly assigned to the experimental or control group. In the experimental group, the LD donor site was dressed using NPWT (Renasys, Smith and Nephew, Oklahoma, USA) with the suction tube in the midline groove. The conventional method of dressing was used in the control group. The LD musculocutaneous flaps were raised using the conventional method. Skin flaps approximately the size of the previous nipple-areolar complex were used in most cases, except for 3 cases in the experimental group and 5 cases in the control group, in which large skin flaps were used. In all cases, 90% of the LD muscle from the entire back was raised. All thoracodorsal nerves were transected, as well as most of the muscle around the pedicle, to prevent involuntary postoperative muscle contraction. Textured round implants with volumes of 175–350 mL (Mentor) were placed underneath the muscle in all cases, except for 1 case in each group. No other special techniques, such as quilting sutures, sealant, or glue, were used.
This work was reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria [13].
Technique
One suction drain was placed underneath the LD donor site skin flap in both groups. The dressing was then placed on top of the closed wound.
In the experimental group, after the donor site wound was closed, gauze dressing was placed upon the wound. The first layer of the adhesive drape sheet was placed over the gauze dressing and the entire dissected field of the LD flaps to prevent skin maceration. A piece of reticulated open-cell foam was trimmed to a size slightly smaller than the adhesive drape sheet, and then the other adhesive drape sheet and the vacuum tube were placed on top of the foam, just as in conventional NPWT dressing. The NPWT was left in place for 3 days with constant pressure between −80 and −125 mm Hg. Subsequently, a conventional pressure dressing using an elastic bandage was put in place.
In the control group, the donor site wound was dressed with gauze and adhesive tape, or a transparent film with a pad. The pressure dressing was put in place using an elastic bandage.
The drain was removed when the drainage volume was less than 30 mL per day. The volume of all seromas and the duration of wound drainage were recorded. Postoperative follow-up was carried out every week in the first month, followed by 3 months, 6 months, and 1 year after surgery. All patients who presented with a symptomatic seroma on the back were treated with percutaneous needle aspiration, and the aspirated volume was recorded.
Outcome measures
Seroma was defined as clinically noticeable fluid collection at the donor site after the drain had been removed. The incidence of seroma formation was the primary outcome. Seromas that developed after the drain had been removed 1–2 weeks after surgery were treated by percutaneous aspiration. The aspirated volume and the number of percutaneous aspirations were recorded. The aspirated seroma volume and the drainage volume from the suction drain were recorded as the total drainage volume.
The secondary outcome measures were the number of percutaneous aspirations and the total percutaneous aspirated volume. All wound complications were also recorded.
Statistical analysis
Data were analyzed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). The Student t-test was used to derive all P-values. Statistical significance was defined at α=0.05.
RESULTS
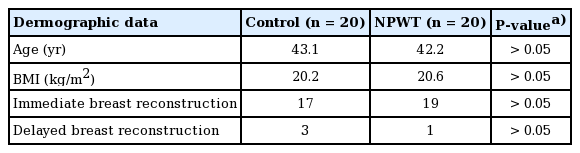
Forty patients were enrolled in the study. Twenty patients were included in each group. All patients received follow-up until 1 year after surgery. There were no statistically significant differences in patient demographic data between the 2 groups (Table 1).
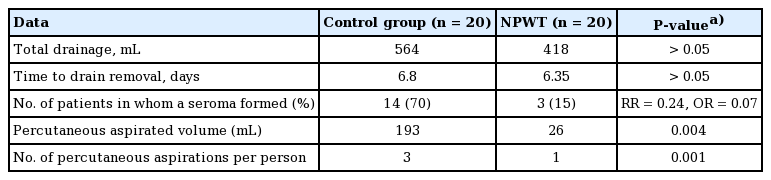
NPWT is shown in Fig. 1. In the NPWT group, the incidence of seroma formation was significantly lower than in the control group (15% vs. 70%; odds ratio=0.07; relative risk, 0.24). Both the mean percutaneous aspirated volume (P=0.004) and the numbers of percutaneous aspirations (P=0.001) were also significantly lower in the NPWT group (Table 2). There were no significant differences in the total drainage volume, the duration of wound drainage, or the length of hospital stay between the NPWT dressing group and the control group (P>0.05).
Negative pressure wound therapy
(A) Donor site area. (B) The donor site wound was closed with gauze dressing, in the same manner as the conventional dressing, and the first layer of the adhesive drape sheet was placed over the gauze dressing and the dissected field of the latissimus dorsi flap to prevent skin maceration. (C) A piece of reticulated open-cell foam was trimmed to a size slightly smaller than the adhesive drape sheet, and then the vacuum tube was placed. (D) Another adhesive drape sheet was applied.
Three patients developed minor skin blebs from the adhesive drape sheet in the NPWT group. They all healed spontaneously after conservative treatment. An infected seroma was found in 1 patient in the control group. She was treated with antibiotics and subsequently healed.
DISCUSSION
Seroma formation at the donor site after the harvest of an LD flap is quite a common complication. Many treatment modalities have been developed in attempts to solve this problem. Schwabegger et al. [5] defined some of possible causes of seroma formation. These mechanisms include the friction of the wound layers and fat necrosis from liberal handling of the electrocautery knife.
The use of quilting sutures (the Chippendale technique) to eliminate dead space at the donor site of an LD flap was first described by Titley et al. [6] in 1997. This method has been reported to be the most effective technique, with an incidence of seroma ranging from 0% to 45.6% [14-17]. However, some minor adverse effects might occur after quilting sutures, such as back pain and limitations of shoulder movement, in addition to the time-consuming nature of the procedure.
The mechanisms of NPWT that contribute to graft stabilization have been well described in the literature, and include limiting shear stresses and totally immobilizing the graft [11]. In this study, we applied NPWT to the donor site of LD flaps in order to limit shear stresses between subcutaneous tissue and the underlying muscle, with the goal of decreasing seroma formation. When the NPWT group was compared with the conventional dressing group, we found that the incidence of seroma formation after drain removal decreased from 70% to 15%. NPWT also reduced the number of percutaneous seroma aspirations from 3 to 1 and decreased the aspirated volume from 193 to 26 mL. However, the total drainage volume was not significantly different between the 2 groups. NPWT is simple to apply, and no other procedures capable of causing discomfort were required. However, NPWT is substantially more expensive than the conventional dressing method. Minor complications, such as skin blebs, may arise from indelicate stripping of the film, but in our study, such complications mostly healed after conservative treatment. There are several limitations of this study. First, the sample size was rather small, and the evaluation of the presence of a seroma was subjective. Second, this was not a blinded study, so potential bias must be considered.
The incidence of seroma formation after drain removal was significantly lower in the NPWT group than in the conventional dressing group. Dressing the donor site with NPWT also reduced the number of percutaneous seroma aspirations and the volume that was aspirated. This study showed that NPWT is a promising tool for reducing the incidence of seroma formation at the donor site after LD flap harvesting. It is a simple and safe technique.
Notes
No potential conflict of interest relevant to this article was reported.