Selection of Implants in Unilateral Prosthetic Breast Reconstruction and Contralateral Augmentation
Article information
Abstract
Background
In breast reconstruction using implants after unilateral mastectomy, it is challenging to create a natural, ptotic contour, and asymmetry is a potential drawback. To achieve breast symmetry and an ideal shape for both breasts, we performed contralateral augmentation in patients undergoing breast reconstruction with implants.
Methods
Patients underwent unilateral mastectomy and 2-stage reconstruction. During the second stage of the procedure, contralateral augmentation mammoplasty was performed. Preoperatively, we obtained the patients’ demographic information, and we then assessed breast volume, the volume and dimensions of the inserted implants, and complications. Breast symmetry was observed by the surgeon and was assessed by measuring the disparity between the final volume of each breast.
Results
Contralateral augmentation was performed in 52 cases. When compared to patients who did not undergo a contralateral balancing procedure, patients who received contralateral augmentation were younger, thinner, and had smaller breasts. During implant selection for contralateral augmentation, we chose implants that were approximately 1 cm shorter in width, 1 level lower in height, and 1 or 2 levels lower in projection than the implants used for reconstruction. The postoperative breast contours were symmetric and the final volume discrepancy between each breast, which was measured by 3-dimensional scanning, was acceptable.
Conclusions
We demonstrate that contralateral augmentation can be recommended for patients who perceive their breasts to be small and not beautiful in order to achieve an ideal and beautiful shape for both breasts. Furthermore, this study offers guidelines for selecting the implant that will lead to the optimal aesthetic outcome.
INTRODUCTION
As breast reconstruction after total mastectomy is commonly performed worldwide, reconstruction techniques using autologous tissue and implants are currently evolving. Previously, the goal of breast reconstruction was to design a breast mound that would allow a patient’s clothes to fit; however, patients’ expectations are now higher, and they want the volume and shape of their breasts to be symmetrical, just as their original breasts were before mastectomy. For this reason, the frequency of contralateral balancing procedures is increasing. Occasionally, moderately symmetric breasts can be achieved by only reconstructing the ipsilateral breast, without performing any procedure on the contralateral side. However, in some cases, such as when the contralateral breast is too large, too small, or too ptotic, it does not have a beautiful and ideal shape, making it difficult to achieve a symmetric volume and contour simply by reconstructing the ipsilateral breast after mastectomy. There are several options for the contralateral balancing procedure, including reduction mammoplasty, augmentation mammoplasty, and mastopexy. Using one of these procedures, a plastic surgeon can transform both breasts into their ideal shape.
Breast reconstruction can be divided into implant-based reconstruction and autologous tissue reconstruction. Each reconstruction method has its advantages and disadvantages, so determining the most suitable method for a patient should be done carefully, taking into consideration the patient’s age, breast contour, body mass index (BMI), underlying disease, and her own desires. Regardless of the method chosen for breast reconstruction, it is not easy to achieve completely beautiful bilateral breasts, and in an effort to achieve symmetry, we are often compelled to operate on the contralateral breast as well. The purpose of a contralateral balancing procedure is to achieve an aesthetically beautiful and natural-appearing breast that is in balance with the opposite side, and through this, the patient can achieve personal satisfaction, improving her self-esteem and quality of life.
Many studies have been conducted of the timing of contralateral balancing procedures; in particular, comparisons have been made between performing a contralateral balancing procedure simultaneously, at the time of initial reconstruction, and performing it as a delayed, second-stage procedure [1-4]. At the authors’ hospital, simultaneous prosthesis-based reconstruction after unilateral mastectomy is most commonly performed. This option is usually preferred by women who want a simple operation and short recovery time, and by those whose chief concern is donor-site scarring. These patients inevitably undergo a secondary operation, during which the previously inserted tissue expander is exchanged for a permanent implant. Therefore, if they have an imperfect contralateral breast and want their breasts to have a more symmetrical appearance, we perform a contralateral balancing procedure at the time of the second operation. Since Korean women often tend to have relatively small breasts, many patients express their desire for augmentation mammoplasty along with a contralateral balancing procedure at the initial preoperative consultation. In this study, we analyzed the patients who underwent contralateral augmentation after breast reconstruction with implants, and evaluated which type of implants allowed the creation of the optimal aesthetic outcomes.
METHODS
Patients and evaluation
The medical records of patients who received implant-based reconstruction by a single surgeon at a single institution were reviewed retrospectively. A total of 188 patients underwent unilateral mastectomy and 2-stage reconstruction using tissue expanders and implants. Patients who received bilateral mastectomy, contralateral prophylactic mastectomy, or a direct-to-implant procedure simultaneously were excluded. The contralateral balancing procedures included augmentation mammoplasty, reduction mammoplasty, and mastopexy. Among these patients, we collected the preoperative demographic information of patients who received contralateral augmentation, and assessed breast volume and complications after the procedure. We also analyzed the volume and dimensions of the inserted implants, including width, height, and projection. We evaluated the aesthetic outcomes at outpatient follow-up visits, based on the findings of the surgeon’s physical examination. In addition, clinical photos were taken and the degree of symmetry was estimated by measuring the discrepancy between the final volume of each side, as assessed by 3-dimensional scanning (Axis Three, AX3 Technologies, Miami, FL, USA).
Surgical procedure
The first stage of the operation was performed simultaneously with the total unilateral mastectomy done by the general surgery team, and we then inserted a tissue expander in the reconstructed breast and slung it with acellular dermal matrix. After sufficient expansion of the skin was achieved by the tissue expander, considering the patient’s desired end volume, the second stage of the operation was performed. Patients who required adjuvant chemotherapy underwent a second operation when the chemotherapy was completed. The existing tissue expander was removed from the ipsilateral breast and a permanent implant was inserted in the dual plane pocket, consisting of submuscular and preexisting acellular dermal matrix. In the contralateral breast, we created a dual plane—of type I, II, or III—according to the degree of ptosis. The augmentation approach was either transaxillary or via the inframammary fold. After inserting salinefilled sizers in both breasts, patients were then placed in a sitting position to confirm the symmetry of size and shape. Subsequently, anatomical silicone gel-textured implants were inserted in both breasts.
RESULTS
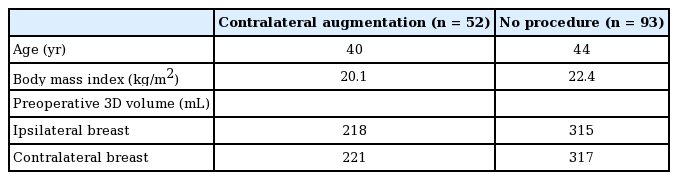
Among the 188 women who received 2-stage, implant-based reconstructions, 93 patients did not undergo a contralateral balancing procedure. Ninety-five patients (50.5%) received a contralateral balancing procedure to create a more beautiful contralateral breast and to improve breast symmetry. Among the patients who received a contralateral balancing procedure, 52 (54.7%) underwent augmentation mammoplasty, 8 (8.4%) underwent reduction mammoplasty, and 35 (36.8%) underwent mastopexy (Fig. 1). Augmentation mammoplasty was the most common contralateral procedure. The mean age of the patients who received augmentation mammoplasty was 40 years, ranging from 30 to 59 years. The mean BMI was 20.1 kg/m2, ranging from 17.21 to 25.86 kg/m2. Most patients were slender and thin, as the BMI of 45 patients (86.5%) was under 23 kg/m2. The mean volume of the preoperatively measured breasts was 218 mL on the side of the lesion, and 221 mL on the healthy side. In contrast, the mean age of the patients who received no contralateral procedure was 44 years, which was older than that of patients who underwent contralateral augmentation. The mean BMI of these patients was 22.4 kg/m2, which was higher than that of patients who underwent contralateral augmentation. The mean volume of the preoperatively measured breasts was also greater, with volumes of 315 mL on the side of the lesion and 317 mL on the healthy side (Table 1). Compared to patients who received no contralateral procedure, patients who received contralateral augmentation mammoplasty were younger, thinner, and had smaller breasts. As their original breasts before mastectomy were not ideally shaped due to insufficient breast volume, they were able to achieve beautiful and properly-sized breasts by simultaneously undergoing contralateral augmentation.
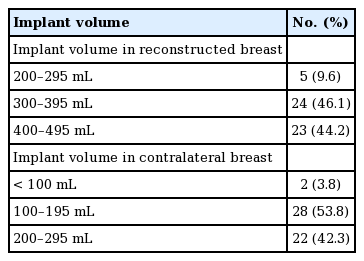
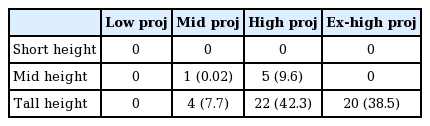
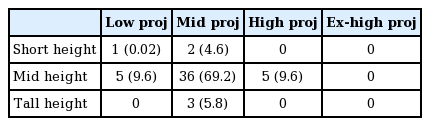
We mainly used anatomical silicone gel-textured implants. Before the second stage of the operation, we had to consider the implant dimensions, including width, height, projection, and volume, to choose the implant that would achieve the optimal results. The average size of the implants inserted into the postmastectomy breast being prepared for reconstruction was 375 mL, ranging from 245 to 495 mL. The average size of the implants that were inserted into the contralateral breast for augmentation was 190 mL, ranging from 90 to 280 mL (Table 2). The operating surgeon chose an implant dimension for the contralateral breast that would be 1 level lower than the implant placed on the post-mastectomy side, taking into consideration each breast’s width, height, and projection. We selected the implant width for the post-mastectomy breast according to the patient’s chest wall width and the width of the preexisting tissue expander. Subsequently, we chose an implant for the contralateral breast, the width of which was approximately 1 cm shorter than that of the reconstructed breast. The average difference in width between each implant in a single patient was 1.35 cm. In terms of implant height and projection, most manufactured implants are divided into 3 levels of height—short, medium, and tall—and 4 levels of projection—low, medium, high, and extrahigh. The surgeon endeavored to select implants for contralateral augmentation that were 1 level lower in height and 1 or 2 levels lower in projection than the implants used for breast reconstruction, a decision that took skin thickness into consideration. The implants that were used for reconstruction were mostly tall in height, and high or extra-high in their projection. The implants that were used for contralateral augmentation were mostly medium-height and medium-projection implants. Tables 3 and 4 show the dimensions of the implants that we used for each breast. On average, the height of the implant used for augmentation was 1.02 levels lower than that of the implant used for reconstruction, and the projection of the implant used for augmentation was 1.45 levels lower than that of the implant used for reconstruction.
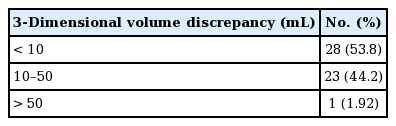
The minimum follow-up period was 3 months, and the mean follow-up period was 11.7 months. Three months after the final operation, clinical photographs and a 3–dimensional scan were taken at the outpatient clinic. The average final volume discrepancy, which was 15.7 mL, was determined by calculating the difference between the 3-dimensionally measured volume of each breast. This is not a noticeable difference to the naked eye, and thus, the results were deemed acceptable (Table 5). The overall satisfaction was high in the evaluation of the operating surgeon according to the patients’ subjective observations (Figs. 2, 3). There were no serious complications from infection, hematoma, or implant malposition; there were only 2 cases involving minor complications among the 52 patients. One was a postoperative infection, which healed well with antibiotic treatment and did not necessitate the removal of the implant, and the other was a malpositioned implant, which was straightforwardly corrected by reposition surgery. Complications requiring reoperation were not reported in any other cases.
A case of a 35-year-old woman
A 450-mL implant, the width of which was 13.0 cm, with tall height and extra-high projection, was inserted into the right breast for reconstruction. A 280-mL implant, the width of which was 12.0 cm with medium height and medium projection, was inserted into the left breast for augmentation. (A–C) Preoperative photographs. The breast volumes measured by 3-dimensional scanning were 150 mL and 156 mL. (D–F) One-year postoperative photographs. The breast volumes measured by 3-dimensional scanning were 462 mL and 464 mL.
A case of a 36-year-old woman
A 410-mL implant, the width of which was 12.5 cm with tall height and extra-high projection, was inserted into the left breast for reconstruction. A 245-mL implant, the width of which was 11.5 cm with medium height and medium projection, was inserted into the right breast for augmentation. (A–C) Preoperative photographs. The breast volumes measured by 3-dimensional scanning were 145 mL and 138 mL. (D–F) Eight-month postoperative photographs. The breast volumes measured by 3-dimensional scanning were 475 mL and 472 mL.
DISCUSSION
Contralateral balancing procedures are commonly performed to achieve symmetry with a reconstructed breast; however, whether it is preferable to perform them during immediate reconstruction or during the delayed second stage is still controversial [1-4]. Some reasons for performing a contralateral balancing procedure during immediate reconstruction are that the second-stage operation can be avoided, and that the time period that patients live with asymmetric breasts (which may cause them to experience depression until the second procedure is performed) can be reduced. However, if a direct-to-implant procedure and contralateral augmentation are performed simultaneously, the remaining skin flap after mastectomy may be at risk when an excessively large implant is inserted at once. Instead, if a contralateral balancing procedure is performed as a delayed operation, patients can determine the preferred size of the implant carefully during the interval between the first-stage operation and the second-stage operation.
In Giacalone’s [5] study, 50% of patients who received delayed reconstruction needed a contralateral secondary procedure to obtain breast symmetry. Losken et al. [3] reviewed 1,394 patients who underwent reconstruction, and found that 67% needed a contralateral symmetry procedure after delayed reconstruction, while 22% needed it after immediate reconstruction. The incidence of a contralateral procedure was higher in cases of implant-based reconstruction than in cases of autologous tissue reconstruction. The most common procedure after implant-based reconstruction was contralateral augmentation, whereas after autologous tissue reconstruction, reduction mammoplasty was the most popular procedure. Implant-based reconstruction required more balancing procedures than autologous tissue reconstruction because it is more difficult to achieve contour symmetry without a secondary procedure in implant-based reconstruction due to its unnaturalness. Nahabedian [2] retrospectively reviewed 382 patients who received breast reconstruction. In that study, balancing procedures were more commonly performed in autologous tissue reconstructions, and they argued that autologous tissue was more amenable than an implant when a secondary procedure was performed.
In Nahabedian and Losken’s study, they performed contralateral balancing procedures as delayed operations; however, in the study of Smith et al. [4], they performed them simultaneously with breast reconstruction. Smith et al. tried to create breast symmetry during the first operation. One of the main advantages of autologous tissue reconstruction is that a second operation can be avoided, but if a second procedure is required, then that advantage disappears. They argued that a single-stage approach could reduce the number of operations, cost of admission and operation, period required for recuperation, and the period that a patient’s breasts remain asymmetric, which can be prolonged when a patient needs adjuvant therapy. However, a disadvantage of implant-based reconstruction is capsular contracture, which can deform the breast shape and lead to asymmetry. Therefore, if a contralateral balancing procedure is performed at the same time as immediate implant-based reconstruction, a new asymmetry will appear later, and then a secondary procedure may be unavoidable.
Surgeons who argue that it is better to offer a contralateral balancing procedure as a delayed, secondary procedure think that if the shape of a breast becomes different from the immediate postoperative result under the influence of postoperative chemotherapy or ongoing fat necrosis, they can consider other surgical options during the second-stage operation. These may include not only the performance of a contralateral procedure, but also an additional procedure in the ipsilateral breast, such as necrotic fat excision, microfat grafting, or inframammary fold repositioning, to achieve a more perfectly balanced breast shape.
In this study, we used 3-dimensional imaging to estimate breast volume and to assess breast symmetry. We took digital photographs and 3-dimensional scans routinely in every patient who underwent breast reconstruction preoperatively, after the first operation, and after the second operation. Many studies have already reviewed 3-dimensional imaging, and it is not 100% accurate; however, its advantage is that we can determine the approximate volume of each breast and estimate the difference between the volume of the breasts, thus determining the amount of reduction or augmentation required in the contralateral breast [6-9].
As other mastectomy options developed, in contrast to the traditional radical mastectomy, the methods and timing (delayed to immediate) of reconstruction also progressed. In the past, delayed reconstruction was widespread, but presently, immediate reconstruction is the more preferred method because it has several advantages. It provides good aesthetic results and psychological benefits, it does not postpone adjuvant therapy, and it does not have a negative effect on patient outcomes. It does not increase local cancer recurrence or affect breast cancer survival [10,11]. However, a reconstructive surgeon should not overlook the remaining oncologic risk on the contralateral side when performing an operation [12]. When there is cancer in one breast, the potential risk that cancer will be found in the contralateral breast in the future is not great, but it still exists, and we cannot ignore it. The likelihood that breast cancer will appear in the contralateral side is 6% after 10 years and 9% after 20 years [13-16]. Therefore, a surgeon should explain this possibility to patients and evaluate the opposite breast for cancer development properly by regular physical examinations, mammography, and magnetic resonance imaging before surgery [17]. Furthermore, a surgeon should recommend regular oncologic surveillance during the postoperative period. It has been suggested that implant-based augmentation has the disadvantage of reducing the sensitivity of mammography, but this usually happens when the implant is inserted in a subglandular plane [18,19]. This can be overcome when the implant is placed under the pectoralis major muscle; in this case, the breast tissue can be stretched by the volume of the implant, and it becomes easier to palpate for the detection of a possible mass. According to previous studies, augmentation mammoplasty as a contralateral balancing procedure does not delay the detection or diagnosis of newly developed cancer and it does not affect the prognosis of cancer [1]. If patients are made aware of the oncologic issue and agree to receive regular cancer screening, a contralateral balancing procedure is an effective operation for breast symmetry that can be recommended.
Patients’ expectations and the desire to achieve breast symmetry after breast reconstruction are increasing. In this study, augmentation mammoplasty was most commonly used as a contralateral balancing procedure because Korean women are more slender and have more hypoplastic breasts than Western women. Performing contralateral augmentation mammoplasty can provide patients with heightened self-esteem and satisfaction, and improve their quality of life through the achievement of breast symmetry. Patients who receive a 2-stage procedure will inevitably need a second operation, so it is recommended to perform the contralateral procedure at the second stage in order to achieve an ideal and beautiful shape in both breasts. Furthermore, this study offers guidelines for the selection of implant dimensions (width, height, and projection) that will achieve the optimal aesthetic outcomes.
Notes
No potential conflict of interest relevant to this article was reported.
Notes
PATIENT CONSENT
The patient provided written informed consent for the publication and the use of their images.