Efficacy of Quilting Sutures and Fibrin Sealant Together for Prevention of Seroma in Extended Latissimus Dorsi Flap Donor Sites
Article information
Abstract
Background
The extended latissimus dorsi flap is important for breast reconstruction. Unfortunately, donor site seroma is the most common complication of extended latissimus dorsi flap for breast reconstruction. Although using fibrin sealant in the donor site reduces the rate of seroma formation, donor site seroma remains a troublesome complication. The purpose of this study was to analyze the effectiveness of the combination of quilting sutures and fibrin sealant in the latissimus dorsi donor site for the prevention of seroma.
Methods
Forty-six patients who underwent breast reconstruction with extended latissimus flap were enrolled in the study. The patients received either fibrin sealant (group 1, n=25) or a combination of fibrin sealant and quilting sutures (group 2, n=21) in the extended latissimus dorsi donor site. Outcome measures were obtained from the incidence, volume of postoperative seroma, total drainage amount, indwelling period of drainage, and duration of hospital stay.
Results
The incidence of seroma was 76% in group 1 and 42.9% in group 2 (P=0.022). We also found significant reductions in seroma volume (P=0.043), total drainage amount (P=0.002), indwelling period of drainage (P=0.01), and frequency of aspiration (P=0.043). The quilting sutures did not affect the rate of drainage, tube reinsertion, or hospital stay.
Conclusions
The use of quilting sutures combined with fibrin sealant on the latissimus dorsi flap donor site is helpful for reducing the overall seroma volume, frequency of aspiration, and total drainage amount.
INTRODUCTION
Latissimus dorsi flap is popular for breast reconstruction because it is well vascularized, stable, and easy to approach. Since Hokin [1] proposed latissimus dorsi flap for breast reconstruction, latissimus dorsi (LD) musculocutaneous flap, extended LD flap, or mini LD flap have progressively been used for early immediate breast reconstruction and delayed breast reconstruction [2,3]. Unfortunately, donor site seroma is the most common complication of latissimus dorsi flap for breast reconstruction. The effective and timely provision of breast cancer treatment is particularly hampered by the development of postoperative seroma in approximately 15% to 81% of patients undergoing surgery [4]. Recently, seroma incidence has been reported to be 6% to 80% in cases of autogenous LD flap reconstruction and LD-implant reconstruction [5-7]. The development of seroma after breast surgery is multifactorial, including a variety of dissection sizes, a result of shearing between subcutaneous tissue and underlying muscle, dead space, leakage from the disruption of the lymphatic and vascular channels, and inflammatory processes [8]. Seroma can be a significant source of a patient's discomfort, anxiety, infection, wound dehiscence, and consequently, flap necrosis, and scars [9,10]. For the prevention of donor site seroma, a variety of treatment measures such as electrocautery, endoscopic harvest, compression garment, repetitive aspiration, sclerotherapy, steroid injection, prolonged drainage, and capsulectomy have been described [7,11]. However, these treatments and preventive measures have not been uniformly successful.
Some studies have reported that fibrin sealant was useful for preventing seroma in a rat model, and the rate of seroma formation had been reduced from 90% to 20% using fibrin sealant [9,12]. Fibrin sealant has been described as a useful agent for reducing seroma after various surgical procedures, skin grafts, and cosmetic procedures [13,14]. Fibrin sealant plays a role as an adhesive agent in wound healing. Fibrin sealant is a mixture of fibrinogen and collagen. When the two solutions are mixed together in the presence of ionized calcium and fibronectin, the thrombin rapidly cleaves the fibrinogen to the fibrin. Fibrin polymers form a fibrin clot that is strengthened by a factor VIII-induced cross-linking [15]. Fibrin sealant decreases dead space, seals open lymphatic channels, achieves rapid hemostasis of large oozing raw surfaces, and adheres two raw surfaces together.
The commonly used modality for preventing seroma is quilting of the LD donor site. The use of quilting sutures to eliminate dead space under the flap has been reported to reduce the incidence of postoperative seroma formation in a variety of surgical procedures [16]. Recently, many studies in breast reconstruction surgery have shown that the use of quilting sutures of the LD donor site is useful in seroma prevention [11,17-20].
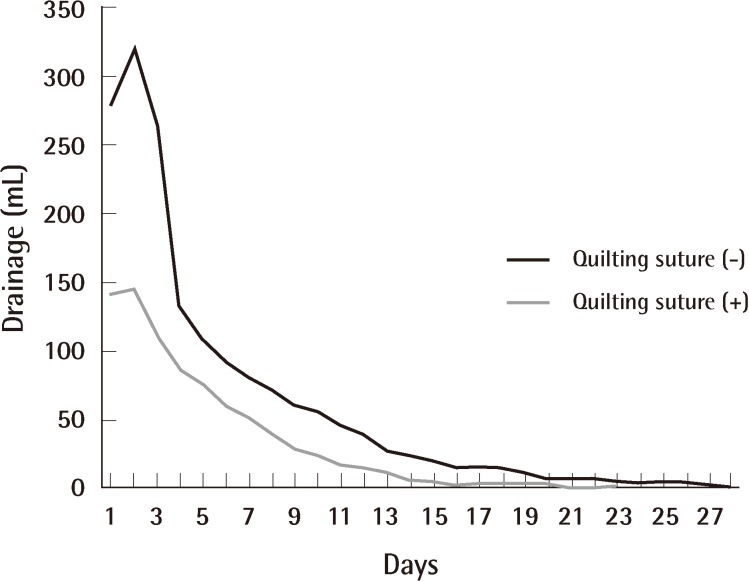
Furthermore, several studies [17-20] have reported that a combination of fibrin sealant and quilting sutures reduced seroma formation and total drainage. However, no comparative studies of an only fibrin sealant group and a combination of fibrin sealant and quilting suture group have been reported in breast reconstruction. We postulated that combining these two modalities could synergistically reduce the seroma rate and drainage volume compared to using fibrin sealant alone.
METHODS
A non-randomized retrospective study was conducted on 46 patients who underwent breast reconstruction with extended latissimus dorsi flaps between August 2010 and September 2011. The control group consisted of 25 patients who underwent breast reconstruction with extended latissimus dorsi flap between November 2010 and March 2011. The experimental quilting suture group consisted of 21 patients who underwent breast reconstruction with extended latissimus dorsi flap between April and August 2011. The patients' charts were reviewed and information regarding age, body mass index (BMI), type of reconstruction, flap size, seroma volume, frequency of aspiration, reinsertion of drain, volume of drainage, indwelling period of drainage, and hospital stay was recorded.
Surgical techniques
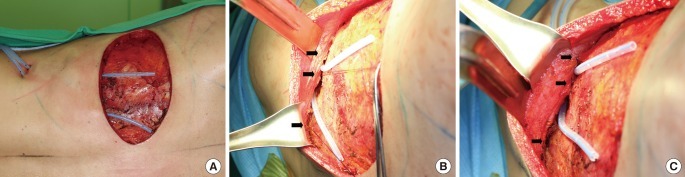
A single surgeon performed the flap harvest and donor site closures in both groups. A transverse skin paddle was included. The extended latissimus dorsi flap size was approximately 2 to 3 cm, largely designed in reference to the removed breast tissue. Dissection of the flap was accomplished using electrocautery with a Colorado tip (Microneedle, ConMed Corporation, Utica, NY, USA) for minimizing thermal injury via an open technique. Adipose tissue was incorporated in the flap. The thoracodorsal nerve was transected, and the flap was transposed anteriorly. After meticulous electrocautery of noticeable donor bleeding, saline irrigation was performed. Two drainage tubes (HemoVAC, 200 mL) were inserted. The location and number of drainage tubes was the same for all patients. The control group (group 1) had the donor site closed with fibrin sealant (Tisseel, Baxter International Inc., Utica, NY, USA). The cavity was evenly sprayed with 4 mL of fibrin sealant using a spray device. Pressure was applied to the skin flaps for 3 minutes to ensure the obliteration of dead space. In the study group (group 2), one row of 2/0 polyglactin (Vicryl, Ethicon Inc., Somerville, NJ, USA) sutures was used at the three points (lateral, middle, medial side) of each skin flap (Fig. 1). Fibrin sealant was applied in the same manner as used in the control group. Both groups had standard postoperative care. All of the volumes and durations of wound drainage were recorded postoperatively. When the drainage was less than 20 mL over a 24-hour period, the drainage tubes were removed. In a postoperative clinical review, all symptomatic donor site seromas were aspirated, and the volumes were recorded.
Outcome measures
The primary outcome measures were the incidence and volume of postoperative seroma. A seroma was defined as the aspirated volume at the donor site above 10 mL or having to perform aspiration at least twice. Aspiration was performed using an aseptic technique; the total volume and frequency were recorded.
Secondary outcome measures were the total drainage, indwelling period of drainage, length of hospital stay, and rate of drainage reinsertion.
Statistical analysis
Patient data were collated and inputted into a spreadsheet (Microsoft Excel 2007, Microsoft, Redmond, WA, USA). Statistical analysis was performed using PASW Statistics ver. 18.0 (IBM Corp., New York, NY, USA), the independent t test (age, body mass index, and indwelling period), Mann-Whitney U test (flap size, volume of seroma, frequency of aspiration, volume of drainage, and hospital stay), Pearson's chi-squared test (seroma rate) and Fisher's exact test (HemoVAC reinsertion rate) were used to analyze the effects of interventions. We assumed that there was statistical significance if the P-value was less than 0.05. All the results were shown as mean±standard deviation or median (interquartile range).
RESULTS
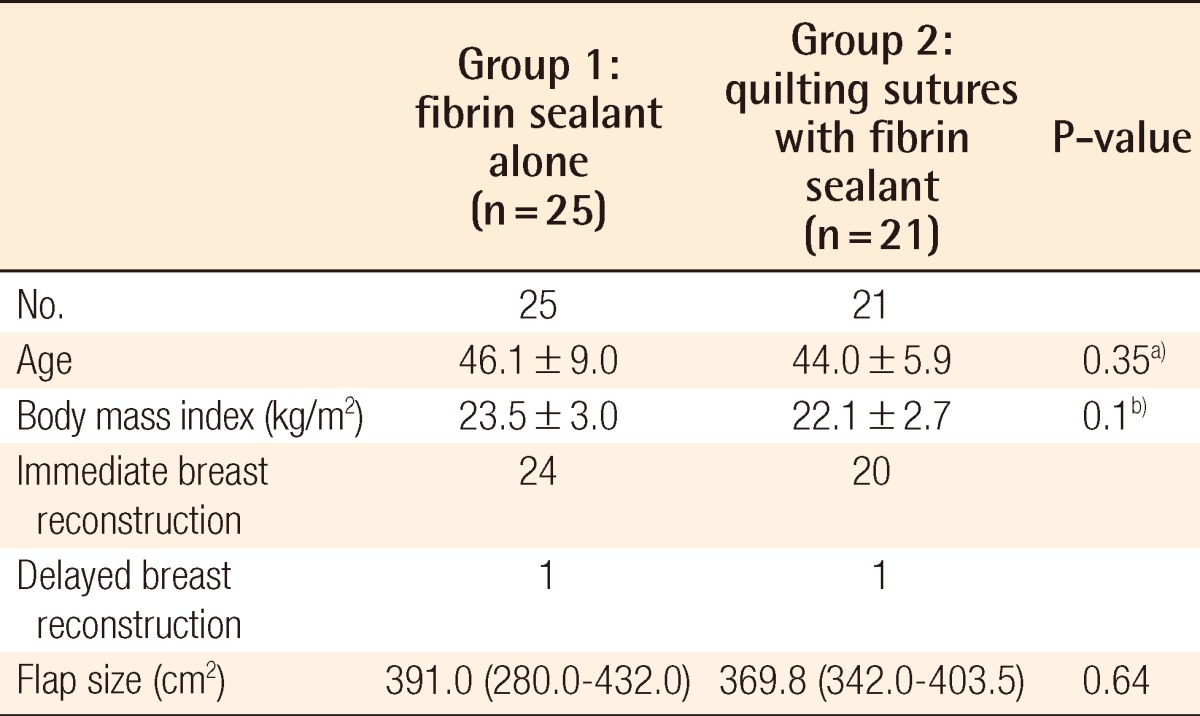
The average age of all the patients was 45 years, the average body mass index was 22.9±2.9 kg/m2, and the average flap size was 362.0±97.1 cm2. There were no statistically significant differences between the two groups with regard to age, body mass index, and flap size (Table 1).
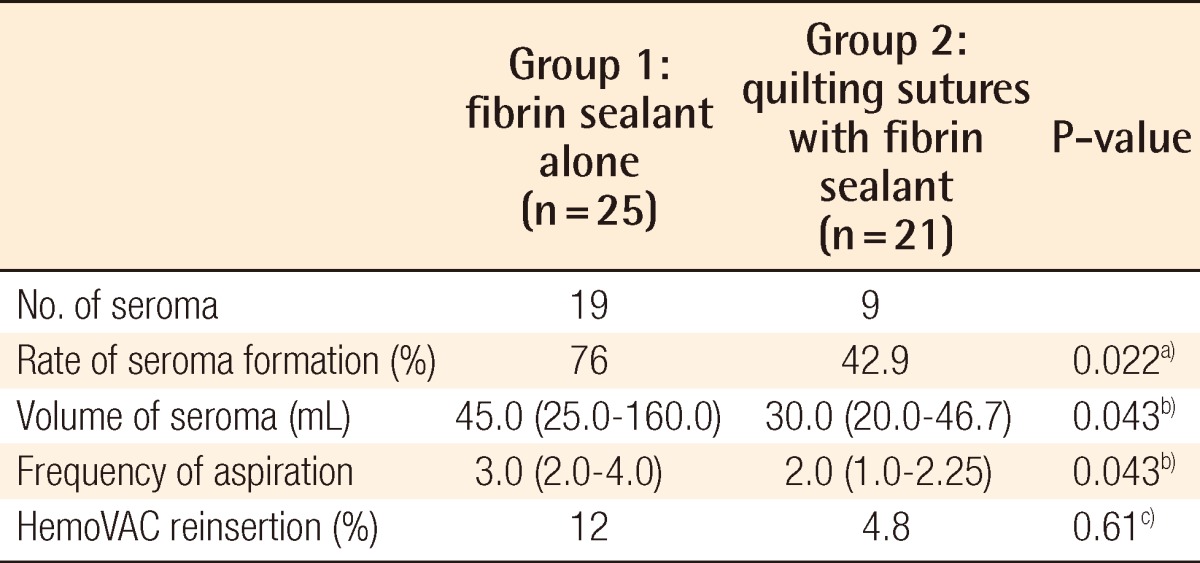
Seroma and drainage
The incidence of seroma was 76% in group 1 and 42.9% in group 2 (odds ratio, 0.24; relative risk, 0.56; P<0.05) (Table 2). The seroma volumes were decreased with quilting sutures from a median of 45.0 mL (25.0-160.0 mL) to 30.0 mL (20.0-46.7 mL) (P=0.022). Quilting sutures reduced the frequency of aspiration from a median of 3.0 (2.0-4.0) times to 2.0 (1.0-2.25) times (P=0.043). However, quilting sutures did not reduce the rate of drainage reinsertion (P=0.61) (Table 2).
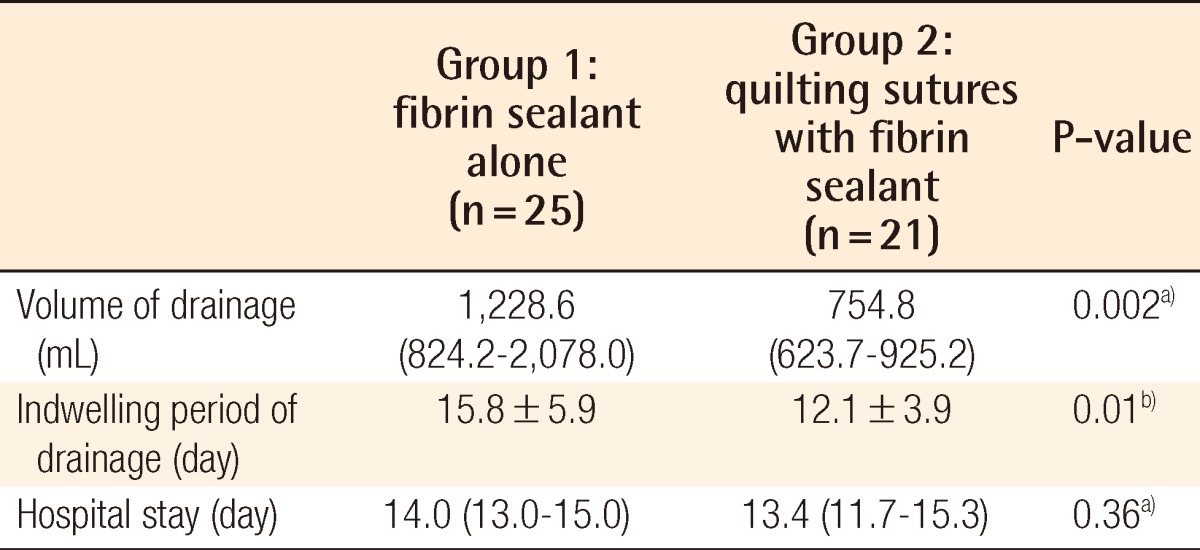
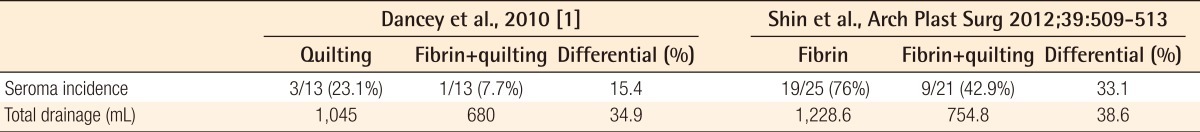
The median total volume of drainage was significantly higher in group 1 (1,228.6 mL [824.2 to 2,078.0 mL]) than group 2 (754.8 mL [623.7 to 925.2 mL]; P=0.002). The mean indwelling period of the drains was 15.8 days in group 1 and 12.1 days in group 2 (P=0.01). However, the period of hospital stay was not statistically significantly different between the two groups (P=0.36) (Table 3). The average daily drainage was consistently lower for group 2 (Fig. 2).
DISCUSSION
The extended latissimus dorsi flap is safe, reliable, and popular for breast reconstruction. However, donor site seroma has been reported in up to 80% of patients who undergo breast reconstruction with extended latissimus dorsi flap [5-7]. Patients who have suffered from seroma need repetitive aspiration in a postoperative clinical review. Occasionally, aspiration fails to remove seromas, which then requires reoperation to facilitate debridement of fibrinous loculations. Prevention of seromas decreases patient morbidity and the additional cost for treatment. The reduction of seroma also avoids delaying adjuvant chemotherapy and radiotherapy.
The cause of seroma seems to be multifactorial, although the etiology of seroma formation remains unknown. Schwabegger et al. [7] suggested that the use of electrocautery is a major causative factor in seroma formation after harvesting a latissimus dorsi flap, and it was postulated that thermal damage to tissue increases the incidence of seroma. We performed electrocautery with a Colorado needle to decrease thermal injury. Even if thermal injury had contributed to seroma formation in our patients, a single surgeon performed the flap harvest, thus this should not affect the group comparison. Taghizadeh et al. [21] reported that immediate breast reconstruction contributed to a higher rate of initial seroma, and they assumed that this resulted from axillary nodal dissection. Jain et al. [22] and Watt-Boolsen et al. [23] suggested that seroma could be plasma filtrates, either in the form of protein-poor transudates or a lymphatic leak. Alternatively, they proposed that it may be secondary to increase capillary permeability, resulting in protein-rich exudates, which are often observed during the inflammatory phase of wound healing. Interestingly, several studies have been shown that drains can act as irritants by prolonging the inflammatory phase, thus contributing to seroma formation [19,21].
Seroma formation occurs from extensive surgical dissection and disruption of tissue that results in a dead space while communicating with other areas of dissection following a mastectomy, axillary lymph node dissection, and LD muscle harvest [5,22,24]. Fibrin sealant and quilting sutures partly aim to restore the integrity of tissue planes and remove dead space. Saltz et al. [13] reported that fibrin sealant used in various surgical circumstances reduced seroma formation. Recently, Ali et al. [19] and Dancey et al. [20] have reported that a combination of fibrin sealant and quilting sutures reduced seroma formation, frequency of aspiration, and length of the drainage period, which was superior to the use of quilting sutures alone. The cost of fibrin sealant is approximately ₩315,000 (about 280USD) for each 4 mL kit. This cost is offset by reduced drainage and postoperative visits. Moreover, the decrease in a patient's inconvenience and discomfort is invaluable.
Titley et al. [11] described a quilting technique performed in 10 patients who underwent a latissimus dorsi harvest. They quilted the skin flaps to the underlying tissue using 2/0 polydioxanone interrupted sutures every 3 to 4 cm in multiple layers. Seroma rates reduced from 56% to 0% after the quilting technique was used. Daltrey et al. [17] reported on a randomized trial of 108 patients who underwent classic and extended latissimus dorsi harvest. They performed multi-layered quilting using 2/0 vicryl interrupted sutures 3 to 4 cm apart in multiple layers. Seroma rates was reduced from 95% to 83%. Following these studies, Gisquet et al. [18] described that quilting sutures were also effective for reducing donor site seroma.
Several authors have presented the shearing effect of skin flaps against the underlying structures and dead space between the two planes [10,11]. Quilting sutures eliminate dead space and shearing forces; their use reduced seroma in our study from 76% to 42.9%.
This is the first study comparing a fibrin sealant only group to a combination of fibrin sealant and quilting suture group. We have shown that the combination of fibrin sealant and quilting suture is significantly superior to fibrin sealant alone for reducing the seroma rate, seroma volume, total drainage amount, and length of drain indwelling period with proportionately fewer aspirations. It also led to a decrease in postoperative visits for aspirations, which decreased the patients' discomfort and inconvenience as well. However, it did not affect the length of hospital stay.
Multidisciplinary preventative strategies for reducing seroma should be designed and implemented depending on the predisposing risk factors. This study proposes that a combination of fibrin sealant and quilting sutures for an extended LD donor site closure may be an effective procedure to avoid donor-site seroma and related morbidity. However, our study is retrospective; thus, a major multicenter randomized controlled trial is required to provide powerful and reliable evidence.
Notes
This article was presented as a poster at the 69th Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 11, 2011 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.