A shark attack treated in a tertiary care centre: Case report and review of the literature
Article information
Abstract
Although uncommon, shark attacks can lead to devastating outcomes for victims. Surgeons also face unique challenges during operative management such as exsanguination, shock, specific injury patterns and infections. This case report presents the management of a 39-year-old previously healthy female attacked by a shark while on vacation in Mexico. The patient sustained severe injuries to her left arm and her left thigh. She was transferred to a Canadian institution after ambiguous operative management in Mexico and presented with no clear antibiotic coverage and a Volkman’s contracture of the left upper extremity. In total, the patient underwent four washouts of wounds, two split-thickness skin grafts, one free anterolateral thigh flap, and one free transverse rectus abdominus myocutaneous flap for the reconstruction and salvage of the left lower extremity. This article highlights the specifics of this case and describes important points in managing these devastating injuries.
INTRODUCTION
Shark attacks evoke popular ideations of fear and curiosity. Although often presented by the media due to their sensational nature, shark attacks remain a relatively rare event [1,2]. Indeed, no more than 50 to 80 attacks on average have been reported annually in the literature [2-4]. The vast majority of these attacks occur at dawn or dusk and involve surfers or windsurfers [1]. Injuries most commonly involve the lower extremity, with the upper extremity being second most commonly injured [1,2]. The attacks occur for a wide variety of reasons ranging from inquisitive attempts to frank predatory attacks (mainly due to mistaken identity of the prey). Attacks can rapidly be fatal if not managed appropriately in the pre-hospital setting. Immediate first aid is essential considering the principal cause of death has been reported as exsanguination and hypovolemic shock from an arterial injury [1,2]. This describes what is to the best of our knowledge the first reported non-fatal shark attack treated at a Canadian institution and the subsequent management challenges encountered. We also review the literature and describe the unique management features of shark injuries to the Canadian plastic surgeon to whom this may not be a familiar injury.
CASE
A 39-year-old healthy woman was attacked by a shark while on vacation, and sustained severe injuries to her left lateral thigh as well as her left arm. The details of management received at the initial treating hospital remain vague however operative procedures performed included the repair of multiple muscles, tendons, and nerve lacerations to the left forearm with closure under tension. In addition, closure of the left thigh wound defect was attempted using the recovered amputated part as a composite graft. No clear record of antibiotic use was available.
Upon arrival six days post injury (PID #6), the left upper extremity was dressed but not splinted. The digits were dusky with areas of skin necrosis, no peripheral pulses were palpable however a weak radial pulse was audible with the use of a hand-held Doppler. The wrist and digits were flexed demonstrating signs of a significant Volkmann’s contracture (Fig. 1). The left lower extremity wound was covered with a bolster dressing under which the necrotic composite graft was present (Fig. 2). There was also copious sero-purulent fluid draining from the wound, in addition to salt water and sand.

Left upper extremity upon arrival to Canada
Left upper extremity status upon arrival to Canada prior to undergoing first Canadian operative management demonstrating Volkmann’s contracture.

Left thigh upon arrival to Canada
Left thigh upon arrival to Canada prior to undergoing first Canadian operative management illustrating a necrotic composite graft.
The patient was admitted, was started empirically on broad spectrum antibiotics (including ancef, flagyl, and clindamycin) and infectious diseases was immediately consulted to help guide therapy while awaiting operative management.
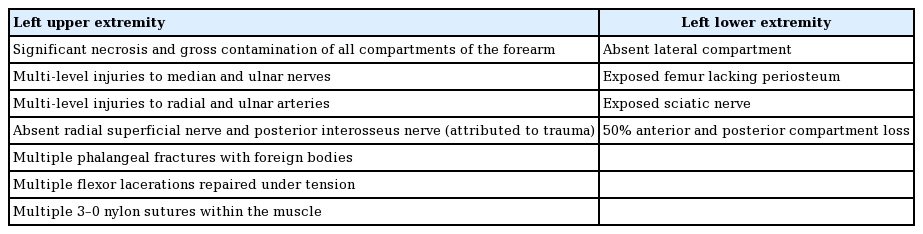
An urgent irrigation and debridement of the upper and lower extremity wounds was performed the day of arrival. Fasciotomies, fascial biopsy, and exploration of the median, and ulnar nerves of the left upper extremity were also performed. Numerous significant injuries were seen (Figs. 3, 4) and are described in detail in Table 1.
Left upper extremity during the initial debridement
A first urgent Canadian irrigation and debridement of the patient’s left upper extremity was undertaken at the time of arrival to our institution to assess the extent of the injuries.
Left thigh during the initial debridement
During the initial urgent Canadian irrigation and debridement, the left thigh was also debrided and assessed for the extent of injuries.
Culture results demonstrated the presence of Candida Glabrata, Bacillus Pumilis, and Bacillus Megaterium. Antibiotic therapy was modified accordingly to include vancomycin, ceftazidime, caspofungin, and flagyl.
A second irrigation and debridement of each site, followed by an anterolateral thigh (ALT) free flap closure of the left thigh defect was performed 48 hours later (PID#9). The postoperative course remained unremarkable up until postoperative day 6 (PID#15) when the flap appeared dusky and cold (Fig. 5) and had a weakening of Doppler signals. An urgent operative exploration was performed and although flow was reestablished across the anastomosis the flap remained unsalvageable. Flap failure is believed to have been caused by thrombosis of the perforator at its entry site into the flap. We hypothesize that the perforator sustained repeated compression injuries between the bare bone edge of the femur and the undersurface of the flap, coinciding with the time of patient’s increased activity and ambulation. A vacuum assisted closure device (VAC) was put in place. Allograft was placed under the VAC to provide a biologic dressing. Integra was subsequently placed over the exposed bone in the left thigh and later successfully covered with a split-thickness skin graft. The patient’s left arm had sustained significant soft tissue defects, Volkmann’s contracture and severe neurovascular injury. On PID#33, the patient was clinically stable and psychologically ready to undergo an elective mid-humeral amputation of the left arm after the left hand remained insensate and perfused only by collateral flow.
Anterolateral thigh flap’s (ALT) congested appearance
The left thigh was reconstructed using a contralateral ALT flap. The status of the flap was stable until postoperative day 6 (PID#15) when, as illustrated, the flap started to appear dusky, cold and had weakened Doppler signals.
On PID#54 the patient was discharged to a rehabilitation center, mobilizing with crutches. Despite adequate functional recovery, the aesthetic result remained unacceptable (Fig. 6) and as a result, on PID#393, a final reconstructive procedure was performed to replace the split-thickness skin graft with a free transverse rectus abdominus myocutaneous flap (TRAM). The delay in performing the TRAM allowed for soft tissue stabilization and the patient to optimize her physical and emotional status in the presence of her family. The patient was discharged home on postoperative day 14 after an uneventful hospital course. An acceptable aesthetic and functional outcome was achieved (Fig. 7). Rehabilitation received during her time in hospital and beyond allowed her to resume daily activities. The patient did not require formal psychosocial support. Her family brought her continuous assistance and encouragement. The patient was able to use this experience as a stepping-stone into becoming a motivational speaker, writer and member of a shark attack survivors group.

Left thigh aesthetic appearance at discharge
The patient’s left thigh had a good functional outcome upon discharge (PID#54) to a rehabilitation center but the aesthetic result was unsatisfactory with split-thickness skin graft coverage.

Left thigh second reconstructive attempt
The left thigh was reconstructed with a transverse rectus abdominus myocutaneous flap and the aesthetic outcome was satisfactory as shown on postoperative day 28.
In total, the patient underwent four washouts (irrigation and debridement) of wounds, two split-thickness skin grafts, one free ALT flap, and one free TRAM flap for the reconstruction and salvage of the left lower extremity (Fig. 8).
DISCUSSION
Shark attacks remain a rare event [3], however, when they do occur the injuries inflicted to patients can be challenging for even the most experienced medical team. The injuries have been compared to those sustained in military conflicts or high-speed motor vehicle collisions [5,6] as there is significant soft tissue loss and often considerable damage beyond what initially appears to be the zone of injury. The mechanism by which the flesh is torn from the victim involves the shark’s serrated upper teeth acting as a saw and its lower teeth clenching on the prey. A stripping action of the soft tissue of its victim ensues but it rarely leads to fracture [5]. Characteristic bite features have previously been identified in a review of 12 cases from Ihama et al. [5]. Shark bites generally display sharp incisions without abrasions, a serrated edge, and triangular or rectangular flaps of skin. Body appendage severance generally leads to an arc shaped pattern. Moreover, teeth can often be found in the victim’s body. It has been noted that shark teeth are brittle and easily fall out during biting actions both in order to generate a more uniform bite force and because there is no ossification present in their jaw line [5].
Victims of shark attacks can present in various extreme states of exhaustion, exsanguination, hemorrhage, hypovolemia and/or near-drowning [6]. Immediate resuscitation as per the ATLS guidelines should be undertaken [6]. The use of a tourniquet for hemorrhage control remains controversial as it can increase venous bleeding and cause significant crush injuries to surrounding structures as well as distal limb ischemia [1]. The use of elevation and pressure is currently recommended for arterial bleeding control [1]. To better assess the level of injury and better estimate patient outcome, a Shark-Induced Trauma Scale has been developed and includes scoring elements such as initial blood pressure, depth and debility of the injury [7]. The sum of all scores leads to five different levels of injury and a descriptive outcome. The Durban classification has also been developed in order to assess prognosis based on wound description by using a three-grade injury scale [6].
As with all trauma, hospital-based management of shark attacks initially involves a trauma assessment based on the ATLS guidelines [1]. Once the patient is stable, operative management for further wound exploration is required to better assess all anatomical structures. Copious irrigation, and debridement of devitalized tissue is also necessary [7]. The first surgical procedure should be short and goal-oriented [1]. Plain radiographs of all injured sites are necessary to better detect possible fracture, fragments of teeth, or periosteal injury [1].
Infection remains one of the most difficult complications following shark attacks. All shark-attack wounds need to be considered as heavily contaminated by sand, debris, and multimicrobial flora. In that regard, 81 different bacteria species have been identified in the oral flora of sharks and some cases have progressed to fulminant necrotizing myositis and necrotizing fasciitis [1,7]. Broad-spectrum empirical antibiotic therapy is recommended for all shark injuries and should cover Vibrio, Aeromonas, Staphylococcus, Streptococcus, and enteric species [6-8]. This can present a major challenge to the reconstructive process, especially considering the atypical organisms often associated with shark injuries [7]. Recommended empiric antibiotic combinations include Tazocin and Ciprofloxacin or Metronidazole with a second-generation cephalosporin [1]. Early involvement of colleagues in infectious diseases to guide antibiotic therapy should be considered as well.
Reconstruction of the wounds will depend on the exact nature of the injury, however standard reconstructive principles apply [9]. Postoperative care following a shark injury is of high importance as in any patient, however specific attention will need to be paid to physical rehabilitation and psychological support.
Notes
No potential conflict of interest relevant to this article was reported.
PATIENT CONSENT
The patient provided written informed consent for the publication and the use of their images.