Volumetric lipoinjection of the fronto-orbital and temporal complex with adipose stem cells for the aesthetic restoration of sequelae of craniosynostosis
Article information
Abstract
Background
Non-syndromic craniosynostosis causes craniofacial asymmetry and may persist after cranioplasty. These postoperative asymmetries are primarily depressions. In some cases, patients may be subjected to pranks and harassment by their peers, affecting their psychosocial development. We propose lipoinjection enriched with adipose stem cells (ASCs) to treat the sequelae of craniosynostosis in the fronto-orbital and temporal complex in cranioplasty patients, with the goal of improving the appearance of the upper third of the face.
Methods
Twelve children (four boys and eight girls) between 4 and 8 years of age (mean age, 6 years) in the postoperative period after treatment for plagiocephaly, brachycephaly, and trigonocephaly were included, with a follow-up period of 1 to 18 months. Fat tissue was obtained from the lower abdomen, and ASCs were isolated using the Yoshimura technique. Lipoinjection was performed using several mini-approaches to ensure adequate distribution.
Results
Two different scales were used to evaluate the aesthetic outcomes. At 6 months, three plastic surgeons independent of the study classified the results using a Likert scale. The patients’ parents categorized the results using a visual analog scale at 6, 9, and 18 months. R esults were favorable on both scales, as the patients’ facial appearance improved and they reported increased happiness and self-esteem due to their remodeled facial appearance.
Conclusions
We suggest that lipoinjection enriched with ASCs is a good alternative for correcting asymmetry of the fronto-orbital and temporal contour in patients with sequelae of craniosynostosis. This treatment will help boost patients’ self-esteem starting at an early age.
INTRODUCTION
Isolated non-syndromic craniosynostosis causes various degrees of craniofacial asymmetry, particularly in cases affecting the coronal and frontal sutures. To date, various surgical techniques have been developed to treat this condition; however, fronto-orbital advancement with frontal remodeling and its variants are the most frequently used. Regardless of the technique that is chosen, some types of asymmetry persist or recur to some degree, especially when the base of the skull is asymmetrical [1-4]. Persing [4] reported that irregularities persisted even after advancement of the fronto-orbital contour, and proposed a second intervention between the ages of 3 and 5 years of age. This would reduce the extent of the deformity, enabling patients to attract less attention from their peers during their early years at school.
Craniofacial malformations undoubtedly have a certain degree of psychosocial effects, as affected preschoolers and elementary school students are likely to be subjected to some degree of harassment. Childhood and adolescence are critical stages in which the role of the social environment is indispensable for the child’s psychological well-being and the development of his or her self-esteem. Lovegrove and Rumsey [5] reported that children in this vulnerable stage are particularly vulnerable to appearance-related comments, teasing, ridicule, and bullying. Recently, other authors have pointed out that facial asymmetry causes psychological alterations that may affect academic performance and the development of the child’s personality [6,7].
We consider that good facial symmetry in patients with craniofacial sequelae will positively influence children’s development and psychosocial integration. Lipoinjection has been widely used as a volumetric filler in recent years in the field of craniofacial surgery, for diseases such as hemifacial microsomia, the sequelae of trauma, and craniosynostosis [8,9]. Recently, several studies have investigated the clinical use of adipose stem cells (ASCs) to enrich autologous fat grafts for volumetric facial filling [10-13].
The fat tissue collected by suction contains not only adipocytes, but also a significant number of cellular elements from the stromal vascular fraction, such as endothelial cells, pericytes, fibroblasts, and ASCs, among others. ASCs and other cells with regenerative characteristics present in the aspirated fatty tissue play an important role in the viability of these grafts [11]. Studies have shown that one of the main advantages of ASCs is the production of growth factors, which have angiogenic and antiapoptotic properties that lead to increased graft survival [9,14,15]. These growth factors increase the capillary density and improve the quality of the graft, thereby contributing to better long-term survival [16].
The purpose of this study was to analyze the use of volumetric lipoinjection supplemented with ASCs to correct mild to moderate asymmetries, mostly depressions, of the fronto-orbital complex and the temporal region as a treatment alternative for aesthetic improvements after surgical treatment in pediatric patients with craniosynostosis.
METHODS
Volumetric lipoinjection supplemented with ASCs was performed in 12 patients (four boys and eight girls), with an age range of 4 to 8 years (mean age, 6 years). Six patients had plagiocephaly (2 right and 4 left), four had brachycephaly, and two had trigonocephaly (Table 1). The surgical protocol included a complete clinical history, analysis of the degree of deformity (to estimate the area and volume for lipoinjection), and photographic assessments during a follow-up period of 1 to 18 months. All patients and guardians provided written informed consent. This study was approved by Institutional Review Board of Universidad Autonoma de Nuevo Leon, Hospital Universitario “Dr. Jose E. Gonzalez” (registration no. CP 14-003). The procedure was completed under balanced general anesthesia on an outpatient basis. The patients, despite their young age, strongly desired to undergo the procedure.
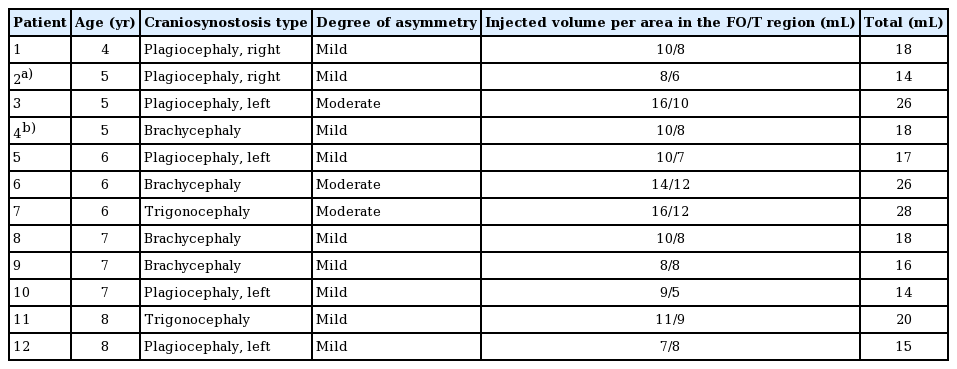
Number of cases with each diagnosis, the degree of asymmetry, the amount injected by area, and the total amount of fat injected
Prior to the procedure, in magnified photos of the patients’ faces, tracing was performed to estimate the volume for infiltration. The lower abdomen was evaluated in each patient as a potential donor site from which to extract the necessary fat. In most cases, the availability of abdominal fat in pediatric patients is limited compared to adult patients, so a more detailed evaluation of the abdomen was necessary to choose an adequate donor site. Cephalexin was prescribed orally the day before surgery and continued for 4 days postoperatively.
Tumescence and fat aspiration
The lower abdomen was infiltrated with a tumescent solution (a dilution of 0.25 mg of epinephrine in 250 mL of saline solution) to harvest adipose grafts. The ratio of infiltration was 1 mL of solution per 1 mL of harvested fat. Fat collection was performed using a blunt-tipped 2-hole cannula 10 cm long and 2.5 mm in diameter attached to a 10-mL Luer-Lock syringe. Manual aspiration was performed because it provides better control and is less traumatic in children. Between 25 and 35 mL of fat was aspirated, and no complications occurred during fat aspiration.
Fat processing technique and isolation of ASCs
The extracted fat was separated into two samples; 10 mL was used for the isolation of ASCs and the remaining sample was enriched with the isolated ASCs and used for lipoinjection. The fatty tissue of the second sample was processed according to the Coleman technique [17]. The sample was centrifuged to remove the hematic/tumescent fraction and the oil layer. ASCs were isolated using the technique described by Yoshimura et al. [14], except for the isolation of stem cells from the fluid [13]. We used the resulting pellet to enrich the fat graft contained in the second sample. Then, 3-mL syringes and a 2-mm blunttipped cannula were used for lipoinjection.
Volumetric lipoinjection technique
A mini-approach was initially performed using a 22-gauge needle. For lipoinjection of the fronto-orbital complex, 2 mini-approaches of 2 to 3 mm were performed in the mid-facial line, one above the hair implant and the other in the glabella to access the supraciliary arches. Another mini-bilateral approach was then made behind the hairline in the temporal fossa (Fig. 1). This was to ensure an adequate distribution of the injected fat (a structural fat graft).
Five-year-old girl with sequelae of craniosynostosis
Intraoperative view of the lipoinjection of adipose stem cells. (A) Glabellar approach. (B) Temporal approach (behind the hairline).
The use of 1-mL syringes and manual pressure provided control and facilitated the use of the necessary volume for infiltration. Lipoinjection was performed using 1.5- to 2.0-mm blunt-tipped cannulas with a single opening near the tip. In the frontal and supraorbital arch, the fat was deposited in the deep subcutaneous layer. This anatomical plane is thin, so the cannula must be directed downward to obtain aesthetic symmetry of the frontal contour, or in unilateral cases, symmetry with the contralateral side. To achieve symmetry, the areas were approached from at least two access sites and the fat graft was deposited using a fanning technique (Fig. 2). The final step consisted of manual manipulation and remodeling of the injected fat, and in some cases, removal of excess grafted fat through the entry site. In the temporal region, fat was deposited between the superficial temporal fascia and the deep temporal fascia. This area is lax and constitutes a displaceable area of the scalp. Overcorrections are usually not needed in this area. All incisions were closed using 4-0 nylon sutures in the scalp and 6-0 nylon sutures in the glabellar region.
RESULTS
The patients were visually evaluated using two scales to assess the aesthetic components of the fronto-orbital and temporal contour. The first scale was applied at 6 months by three plastic surgeons who were not involved in the procedures and were blinded to who performed the procedure. The results were categorized using a Likert scale as excellent, very good, good, or poor. The results were very good in 75% of cases, good in 17%, and poor in 8% (Fig. 3). Patients were also evaluated by their parents using a visual analog scale at 6, 9, and 18 months, and the results were classified as very satisfied, satisfied, slightly satisfied, and unsatisfied. These results were similar to those of the surgeons’ evaluations (Fig. 4). Lipoinjection greatly improved the appearance of the fronto-orbital complex and temporal area. The parents reported feeling more content with their children’s facial appearance.

Likert scale
Likert scale results of postoperative evaluations by three independent plastic surgeons.
Postoperative evaluations using a visual analog scale
Results of the parents’ postoperative evaluations using a visual analog scale at 6 months (A), 9 months (B), and 18 months after the procedure (C).
The injected fat showed adequate permanence, as was documented in photographic assessments used to monitor the medium- and long-term results (Figs. 5, 6). At the 9-month follow-up, the parents rated the results as satisfactory in seven cases (58%), slightly satisfactory in three (25%), and unsatisfactory in two (17%). In the two cases that were deemed to have unsatisfactory results, approximately 50% of the depression had returned. In both cases, a second lipoinjection was performed with very good results, which were rated as satisfactory by the parents, who had positive expectations. The results of the last evaluation (18 months) were satisfactory in eight cases (67%) and unsatisfactory in the remaining four cases (33%). In two of the cases with unsatisfactory results, the parents requested a new intervention, which increased their level of satisfaction. No intraoperative or postoperative complications occurred at the recipient or donor sites.
Five-year-old girl with sequelae of right plagiocephaly
(A) Preoperative view. (B) One month after adipose stem cell lipoinjection. (C) Eighteen months after adipose stem cell lipoinjection.
DISCUSSION
Autologous fat transfers have proven to be an excellent component of craniofacial reconstructive procedures in cases of soft-tissue atrophy. To our knowledge, no reports have specifically investigated lipoinjection enriched with ASCs for aesthetic purposes in the fronto-orbital and temporal contour in pediatric patients. However, Laurent et al. [8] reported a series of nine clinical cases treated with lipoinjection without the use of ASCs in patients with sequelae of craniosynostosis. Of these patients, four required a second intervention and two needed a third lipoinjection.
The reported results regarding the medium- and long-term permanence of facial lipoinjection, as well as lipoinjection in other anatomical areas, are highly variable. In a study conducted almost 3 decades ago, Horl et al. [18] found a mean injected facial fat reabsorption of 49% at 3 months of follow-up and 55% at 6 months, without further loss at 9 and 12 months. However, other authors have reported that fat reabsorption continued between 9 and 14 months of follow-up, and that after 16 months only 32% was still present [19,20]. These reports were of simple lipoinjections without stem cell enrichment.
It is important to mention that there were anatomical differences among the treated areas in our clinical study. The most important anatomical consideration was the thinness of the soft tissues and their intimate relation with the skull. Similarly, anatomical knowledge of this area and its surgical clinical correlations was of vital importance [21,22]. On the basis of a thorough understanding of this area, we carefully carried out lipoinjection of the fronto-orbital complex, injecting into the deep subcutaneous plane and avoiding intradermal lipoinjection, in order to fill in the depressed area while simultaneously avoiding swelling.
During the follow-up period of our study, 33% of patients required a second procedure. In our series, no postoperative imaging studies were performed due to economic considerations. Therefore, based on previous reports, our learning curve, and considering that visual assessment was utilized for follow-up, we determined that a follow-up period of 6 to 9 months after lipoinjection would be appropriate to determine whether a second round of lipoinjection was required.
Recent studies have reported that the presence of postoperative sequelae of facial defects, including post-traumatic alterations, can have a negative psychological impact on affected individuals during social interactions. This may occur during the early school years, primarily due to teasing and harassment by the peers of affected children, influencing their self-esteem and causing sadness, depression, and deterioration in their academic performance [7,23]. Therefore, it is important to offer aesthetic alternatives that may improve social development and prevent negative remarks and jokes during childhood.
Although no self-esteem assessments were performed in this study, most patients were very eager for the procedure to be performed and reported feeling happier about their facial appearance after the procedure.
In this study, we found that lipoinjection was a good alternative to improve the appearance of the fronto-orbital and temporal complex in patients with sequelae of craniosynostosis, or simply to further refine the results obtained after the primary procedure. Facial image plays an important role in the development of self-esteem. We feel that these treatments improved patients’ facial appearance, thereby boosting their self-esteem.
The purpose of these procedures was to improve the balance of the upper third of the face. Adequate medium- and long-term assessments are necessary. The technical approach we propose is a low-risk, minimally invasive procedure that allows a quick recovery and return to daily activities. It is a reproducible option that can be performed in an average time of 2.5 hours, which makes it relatively inexpensive.
While it is true that the evidence available regarding ASC-enriched fat injections suggests that they may have greater permanence, it is important that patients understand that the procedure may need to be repeated for better results. Finally, it is important to note that it would be desirable to include imaging studies in subsequent cases to improve the assessment of medium- and long-term outcomes.
Acknowledgements
The authors thank Sergio Lozano-Rodriguez, M.D. and Alejandro Quiroga-Garza, M.D. for their help in translating the manuscript. We also thank the graphic designer, Ricardo Vela, for his help in making the images presented in this paper.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Universidad Autonoma de Nuevo Leon, Hospital Universitario “Dr. Jose E. Gonzalez” (registration no. CP 14-003) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.