Weight analysis of mastectomy specimens and abdominal flaps used for breast reconstruction in Koreans
Article information
Abstract
Background
Slim patients or those with large breasts may be ineligible for breast reconstruction with an abdominal flap, as the volume of the flap may be insufficient. This study aimed to establish that abdominal tissue–based breast reconstruction can be well suited for Korean patients, despite their thin body habitus.
Methods
A total of 252 patients who underwent postmastectomy breast reconstruction with an abdominal flap from October 2006 to May 2013 were retrospectively reviewed. The patients’ age and body mass index were analyzed, and a correlation analysis was performed between the weight of the mastectomy specimen and that of the initial abdominal flap.
Results
The average weights of the mastectomy specimen and initial abdominal flap were 451.03 g and 644.95 g, respectively. The ratio of the weight of the mastectomy specimen to that of the initial flap was 0.71±0.23. There was a strong positive linear relationship between the weight of the mastectomy specimen and that of the initial flap (Pearson correlation coefficient, 0.728). Thirty nulliparous patients had a final-to-initial flap weight ratio of 0.66±0.11. The 25 patients who underwent a contralateral procedure had a ratio of 0.96±0.30. The adjusted ratio of the final flap weight to the initial flap weight was 0.66±0.12.
Conclusions
Breast weight had a strong positive relationship with abdominal flap weight in Koreans. Abdominal flaps provided sufficient soft tissue for breast reconstruction in most Korean patients, including nulliparous patients. However, when the mastectomy weight is estimated to be >700 g, a contralateral reduction procedure may be considered.
INTRODUCTION
Refinements to available breast reconstruction techniques have contributed to the continued popularity of postmastectomy breast reconstruction [1]. The decision to perform a specific reconstruction is multifactorial, and the patient’s preferences, risk factors, and physical characteristics must be considered [2].
The feel and shape of abdominal flaps adequately mimic the quality of breast tissue. Thus, of the various breast reconstruction methods available, abdominal flaps have been considered the best option for mimicking the natural shape and feel of the breast mound [3-5]. This trend is also seen in Korean patients, who are often reluctant to have a large artificial implant in their body. Although implant-based breast reconstruction can result in outcomes comparable to those of autologous breast reconstruction, an implant cannot surpass the advantages of a lower abdominal flap, including its ability to create a ptotic, naturally shaped breast.
However, some patients are considered poor candidates for breast reconstruction with a lower abdominal flap [6]. For slim patients or those with large breasts, the volume of the transverse rectus abdominis myocutaneous (TRAM) or deep inferior epigastric artery perforator (DIEP) flaps may be insufficient [7]. Generally, Korean patients have a lower body mass index (BMI) and less fat tissue in the lower abdomen. Thus, the misconception exists that Koreans are unsuitable for breast reconstruction with an abdominal flap.
In practice, however, surgeons can perform breast reconstruction with a lower abdominal flap in most patients. If autologous reconstruction is considered the best option for a patient despite a thin body habitus, the use of a DIEP or TRAM flap can be feasible. This study aimed to establish that abdominal tissue–based breast reconstruction can be well suited for Korean patients with thin body habitus. To prove our hypothesis, we investigated the relationship between breast size and abdominal flap weight.
METHODS
Our Institutional Review Board approved this study. Data were collected and reviewed from 252 patients who underwent postmastectomy breast reconstruction with a lower abdominal flap from October 2006 to May 2013. All patients were Korean and lived in the Republic of Korea. Abdominal flaps are abdominally-based free flaps, including free TRAM, DIEP, and superficial inferior epigastric artery (SIEA) flaps. All operations were performed by a single surgeon (J.S.E.), and all patients underwent immediate postmastectomy breast reconstruction. Patients with delayed breast reconstructions were excluded because we could not precisely determine the weight of their previous mastectomy specimen. Neither patients who underwent immediate reconstruction after breast-conserving surgery (BCS) nor patients with a history of BCS were included in the study population. Patients with a history of liposuction were excluded from the study because their abdominal volume would not correspond to that of the general population.
Age and BMI data were collected from the patients’ medical records. The weights of the mastectomy specimen, initial abdominal flap, and the tissue removed from the flap were measured in the operating room. The final flap weight was calculated as the difference between the initial abdominal flap and the removed flap.
Similarly, in patients with no history of parity (delivery), the weights of the mastectomy specimen, initial abdominal flap, and final flap were analyzed. Twenty-five patients underwent reduction mammoplasty for the contralateral breast. The decision to reduce the breast size was made by the patients for aesthetic purposes (e.g., ptotic shape) and functional reasons. The weights of the mastectomy specimen, initial abdominal flap, and final flap were also analyzed in this group.
Preoperative planning and flap insetting
The same principles of flap design were applied in all patients. Reliable perforators were identified using computed tomography angiography, and 1 to 3 dominant perforators were included. The upper margin of the flap was first determined along the upper border of the umbilicus, and the lower margin of the flap was determined by performing pinch and pull-down tests to maximize the flap height. The lateral margins were designed to the waist edge.
In insetting the flap, the authors used the vertical inset method. The side of the flap where the umbilicus is placed is placed on the lateral side and the pubic side of the flap is placed medially. In cases of a contralateral pedicle, the lowest point of the flap is zone II, and zone III goes to the uppermost part. With an ipsilateral pedicle, zones I and III go to the lower pole and zone II fills the upper part of the breast [8].
Statistical analysis
Correlation analysis with the Pearson correlation coefficient was performed between the weight of the mastectomy specimen and that of the initial abdominal flap. The same analyses were also performed between BMI and the weight of the mastectomy specimen and between BMI and the initial flap weight. Continuous variables in the groups with free TRAM and DIEP flaps were compared using the Mann-Whitney test if the data did not have a normal distribution. All reported P-values are 2-sided, and P-values <0.05 were considered to indicate statistical significance. All statistical analyses were performed using the IBM SPSS Statistics version 20 (IBM Corp., Armonk, NY, USA).
RESULTS
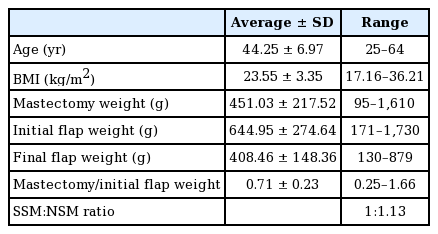
Among the 252 patients, DIEP or SIEA flaps were used in 169 patients (DIEP, 144; SIEA, 15) and muscle-sparing free TRAM flaps were used in 83 patients. The baseline data are summarized in Table 1. The patients’ average age was 44.25±6.97 years (range, 25–64 years), and their average BMI was 23.55 kg/m2 (range, 17.16–36.21 kg/m2). The average mastectomy weight was 451.03 g (range, 95–1,610 g), and the average initial abdominal flap weight was 644.95 g (range, 171–1,730 g). The average weight of the final flap was 408.46 g, and the ratio of the weight of the final flap to that of the initial flap was 0.65±0.11. The ratio of the weight of the mastectomy sample to that of the initial flap was 0.71±0.23.
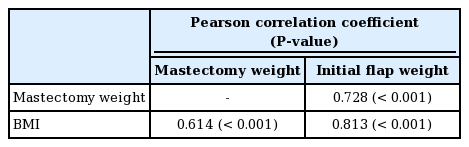
A strong correlation was observed between the weight of the mastectomy specimen and the weight of the initial abdominal flap (Pearson correlation coefficient, 0.728) (Table 2, Fig. 1). BMI had a strong, positive, linear relationship with the mastectomy specimen weight (Pearson correlation coefficient, 0.614) (Fig. 2) and the initial abdominal flap weight (Pearson correlation coefficient, 0.813) (Table 2, Fig. 3).
Relationship between initial flap and mastectomy weight
A strong positive linear correlation was found, with a Pearson correlation coefficient of 0.728 (P<0.001).
Relationship between BMI and mastectomy specimen weight
A strong positive linear correlation was found, with a Pearson correlation coefficient of 0.614 (P<0.001). BMI, body mass index.
Relationship between BMI and initial flap weight
A strong positive linear correlation was found, with a Pearson correlation coefficient of 0.813 (P<0.001). BMI, body mass index.
There were 30 patients with no history of parity (Figs. 4, 5). Their average age was 39 years, and their average BMI was 22.37 kg/m2. The average mastectomy specimen weight in these patients was 380.80 g, and the average initial abdominal flap weight was 547.60 g. The average final flap weight was 345.03 g. The ratio of the weight of the final flap to that of the initial flap was 0.66±0.11.
Results of a 35-year-old female nulliparous patient
The body mass index of the patient was 21.58 kg/m2 at the time of the operation. The oncologic breast surgeon performed nipple-sparing mastectomy for a phyllodes tumor of the right breast. The weight of the excised breast was 415 g. The initial flap weight was 541 g and the final weight was 349 g. (A) Preoperative view. (B) Postoperative view at 7 months of follow-up.
Results of a 32-year-old female nulliparous patient
The body mass index of the patient was 20.4 kg/m2 . The oncologic breast surgeon performed skin-sparing mastectomy. (A) Preoperative view. (B) Postoperative view at 6 months of follow-up. (C) Postoperative view at 12 months after nipple reconstruction.
In the 25 patients who underwent contralateral reduction mammoplasty, the average mastectomy specimen weight was 723.04 g and the average initial abdominal flap weighed 779.88 g. The mean weight of the reduction volume in patients who underwent a contralateral reduction procedure was 233.63±145.12 g. The ratio of the weight of the mastectomy specimen to that of the initial flap was 0.96±0.30. The ratio of the weight of the final flap to that of the initial flap was 0.66±0.12, which was adjusted based on the contralateral reduced breast.
The ratios of the weight of the mastectomy specimen to that of the initial flap in all patients, nulliparous patients, and patients who underwent a contralateral procedure are presented in Fig. 6.
Average ratio of mastectomy to flap weight
The average ratio of the mastectomy weight to the initial flap weight was 71% for all patients. Patients with no history of parity had a smaller ratio (66%) than the total sample of patients; however, this difference was not significant. In patients who underwent a contralateral procedure, the ratio was 96%. However, the abdominal flap provided a matching volume after breast reduction.
DISCUSSION
The importance of patient selection is becoming increasingly appreciated as a predictor of good outcomes after mastectomy and reconstruction. Many variables should be considered during decision-making. Relevant patient-related variables include breast characteristics, obesity, history of abdominal operations, comorbidities, and the patient’s expectations [9-12]. Accordingly, many surgeons hesitate to use an abdominal flap for breast reconstruction in slim or thin patients. The autologous tissue reconstructive procedure most commonly performed in these patients has typically been a latissimus dorsi flap combined with an implant. Other sources of tissue, such as the buttock or thigh, have also been used [13-17].
Korean women are generally considered to be thinner than women in other populations, and consequently have a small abdomen [9]. The mean BMI of the patients in our study was 23.55 kg/m2, which may be considered unusual from the standpoint of Western physicians who might think that Koreans are not good candidates for breast reconstruction with an abdominal flap [18]. In an analysis of 1,303 breast reconstruction procedures with free tissue transfer by Fischer et al. [19], the mean BMI of patients who underwent reconstruction with an autologous free flap was 27.5±5.6 kg/m2, which is significantly higher than the BMI of our patients. Paradoxically, however, the most commonly used method for breast reconstruction in Korea involves a TRAM or DIEP flap [9,20]. Although aversion to artificial materials and reluctance to undergo multiple operations may be an explanation for this trend, a lower abdominal flap is still successfully used for most cases of breast reconstruction, with good satisfaction for both patients and surgeons [21-23].
As our results demonstrated, patients with a small abdomen tended to have small breasts, whereas patients with large breasts tended to have a larger abdomen. Furthermore, the ratio of the weight of the mastectomy specimen to that of the abdominal flap was 0.71, which means that the abdominal flap was large enough to provide the matching volume for a symmetric breast reconstruction even after discarding the poorly perfused zone [22,23]. This tendency was also observed in patients with no history of parity. An abdominal flap can therefore be recommended as the first-line option for breast reconstruction in nulliparous patients.
For patients who underwent contralateral breast reduction, the weight of the mastectomy specimen was almost the same as the abdominal flap weight (Fig. 5). If surgeons have to reconstruct the same-sized breast without contralateral reduction, they may require other strategies, such as the supercharge or turbocharge technique with a bipedicled DIEP flap [24]. Fortunately, most patients with a mastectomy weight of about >700 g hope to have smaller breasts than their original breast size. This means that in most cases, an abdominal flap can provide enough volume to produce the patients’ desired breast size.
One of the limitations of our study was that we analyzed the weight of the specimen and flaps, instead of the volume. Although an analysis with volume measurements may have been more valuable, it is not easy to measure the volume of a flap under sterile conditions. However, considering that the density of breast tissue has been reported to be 0.9954 g/cm3, whereas the density of TRAM flaps was found to be 0.894 g/cm3 [25], the two tissues have almost the same density. Thus, it is still meaningful and practical to compare the weights of the mastectomy specimen and abdominal flap, and comparing the volume based on weight is a reliable approach. Another limitation was the retrospective nature of this study. The surgeon’s selection bias might have played a role because extreme or unfavorable cases for abdominal flap reconstruction might have been excluded when choosing the method of breast reconstruction. Lastly, this study was limited to the Korean population; thus, the results cannot be generalized to all Asian populations. There may be differences among patients living in Central Asia, South Asia, and East Asia.
In conclusion, breast weight had a strong positive relationship with abdominal flap weight in Koreans. TRAM and DIEP flaps alone provided sufficient tissue for breast reconstruction, except when the patients’ mastectomy weight was roughly >700 g. Thus, if patients desire autologous tissue breast reconstruction, abdominal flaps can be a feasible option in most Korean patients, including nulliparous patients.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
This study was approved by the Institutional Review Board of Asan Medical Center (IRB No. 2018-0031) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.