National perioperative outcomes of flap coverage for pressure ulcers from 2005 to 2015 using American College of Surgeons National Surgical Quality Improvement Program
Article information
Abstract
Background
Complication rates after flap coverage for pressure ulcers have been high historically. These patients have multiple risk factors associated with poor wound healing and complications including marginal nutritional status, prolonged immobilization, and a high comorbidities index. This study utilizes the National Surgical Quality Improvement Program (NSQIP) to examine perioperative outcomes of flap coverage for pressure ulcers.
Methods
Data from the NSQIP database (2005–2015) for patient undergoing flap coverage for pressure ulcers was identified. Demographic, perioperative information, and complications were reviewed. One-way analysis of variance and Pearson chi-square were used to assess differences for continuous variables and nominal variables, respectively. Multivariate logistic regression was performed to identify independent risk factors for complications.
Results
There were 755 cases identified: 365 (48.3%) sacral ulcers, 321 (42.5%) ischial ulcers, and 69 (9.1%) trochanteric ulcers. Most patients were older male, with some degree of dependency, neurosensory impairment, high functional comorbidities score, and American Society of Anesthesiologists class 3 or above. The sacral ulcer group had the highest incidence of septic shock and bleeding, while the trochanteric ulcer group had the highest incidence of superficial surgical site infection. There was an overall complication rate of 25% at 30-day follow-up. There was no statistical difference in overall complication among groups. Total operating time, diabetes, and non-elective case were independent risk factors for overall complications.
Conclusions
Despite patients with poor baseline functional status, flap coverage for pressure ulcer patients is safe with acceptable postoperative complications. This type of treatment should be considered for properly selected patients.
INTRODUCTION
Although pressure ulcers are considered a “never event” in healthcare, they are still widely prevalent, with approximately 2.5 million patients treated annually [1,2]. These patients typically have many medical comorbidities, and the elderly, the acutely ill, or those with hip fracture or spinal cord injuries are particularly susceptible to developing pressure ulcers [3-9]. These associated conditions are not only risk factors for pressure ulcer development, but can also affect the healing process following surgical management, leading to a high incidence of wound dehiscence and ulcer recurrence [7-14]. From a healthcare finance perspective, this disease entity has been recognized as being responsible for $9.1–11.6 billon per year in costs, which reflects the long-term nature of this problem as well as recurrence and complications [15,16]. As such, identification of optimal treatment strategies for each individual patient, based on risk factors and surgical outcomes, is necessary.
Treatment of pressure ulcers has evolved over time, transitioning from methods of primary closure and skin grafting to flap reconstruction [17-19]. Current studies on pressure ulcer management focus on long-term follow-up given that the pathophysiological mechanisms of ulcer formation and recurrence require a significant duration of time. These studies report risk factors consisting of low body mass index, active smoking and ischial pressure ulcers [6-14]. The risk factors and complications in the perioperative period have been less well described, with two notable national studies, one on general pressure ulcer management and one specifically for flap coverage [13,14]. Given the difficulties of performing reconstructive flap procedures in patients with comorbidities and chronic, open wounds, it is important to fully recognize the perioperative outcomes associated with the index procedure, independent of complications due to passage of time.
We aim to investigate the risk factors and 30-day perioperative profile of flap coverage for ischial, sacral, and trochanteric pressure ulcers on a national scale using data from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). A secondary aim is to assess differences between pressure ulcers based on region.
METHODS
Patient selection
Using ACS-NSQIP database, patients who underwent pressure ulcer debridement and myocutaneous flap reconstruction as the principal procedures between 2005 and 2015 were identified using principal Current Procedural Terminology codes. Patients were further subgrouped based on location of pressure ulcer: (1) sacral, (2) ischial, and (3) trochanteric. Patient demographics, perioperative information, and postoperative outcomes were compared among the three groups. Postoperative outcomes under consideration included wound dehiscence, infection which included superficial surgical site infection (SSI), deep SSI, organ space SSI, sepsis, septic shock, urinary tract infection, bleeding requiring transfusion, deep vein thrombosis (DVT), pulmonary embolism (PE), flap or graft failure, length of stay (LOS), and readmission and reoperation related to primary procedure. Cumulative complications such as infection and overall complication were counted per patient.
Statistical analysis
All analyses were performed using IBM SPSS version 24.0 (IBM Corp., Armonk, NY, USA). The one-way analysis of variance was used to assess difference in mean for continuous variables and the Pearson chi-square test was used to determine the difference in proportions for binary variable between groups. Univariate analysis was performed to compare patients in different groups for each risk factor. Variables with unadjusted P-value <0.25 from univariate analyses were entered into multivariate logistic regression models to identify independent risk factors for primary adverse outcomes of overall complications, infection, and wound dehiscence for each subgroup and the overall population. Odds ratio (OR) and its 95% confidence interval (CI) for each independent risk factor were derived. All tests were two-tailed, and statistical significance was determined by a P-value <0.05.
RESULTS
Overall patient characteristics and complication profile
There were 755 cases of flap coverage for pressure ulcers identified; 365 (48.3%) for sacral ulcers, 321 (42.5%) for ischial ulcers, and 69 (9.1%) for trochanteric ulcers. Most patients were older, malnourished white males (mean age, 57 years; mean albumin, 2.7 g/dL; male, 468 [62%]; white, 478 [63.3%]), with some degree of dependency (dependent n=522, 69.1%), neurosensory impairment (paraplegia n=143, 18.9%; quadriplegia n=67, 8.9%; hemiplegia n=21, 2.8%), high functional comorbidities score, and American Society of Anesthesiologists (ASA) class 3 or above (n=692, 91.6%). The most prevalent comorbidities included diabetes mellitus (DM; n=219, 29%), hypertension (HTN; n=387, 51.3%), and smoking (n=150, 19.9%) (Table 1).
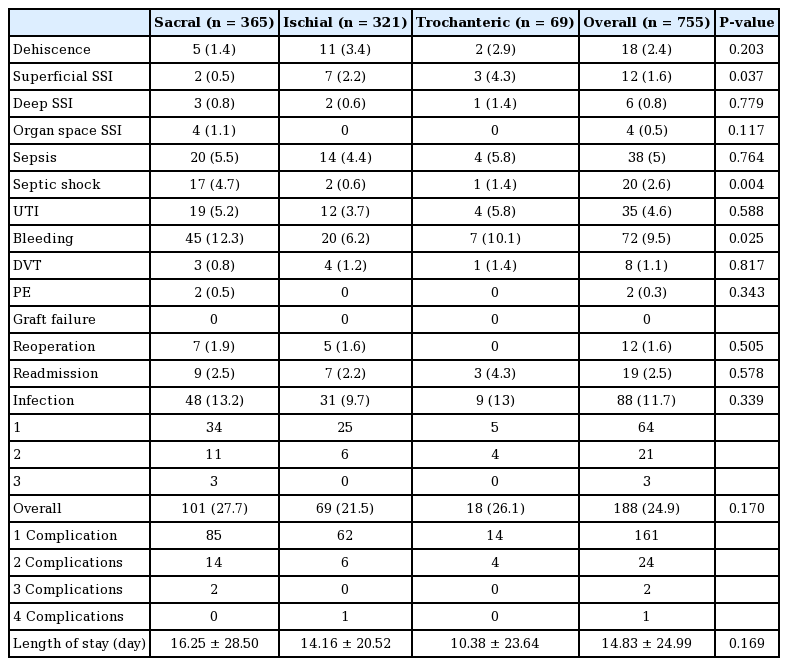
The overall 30-day complication rate was 25%. Individual complications included wound dehiscence (2.4%), infection (11.7%), bleeding requiring transfusion (9.5%), DVT (1.1%), PE (0.3%), reoperation related to principal procedure (1.6%), and readmission related to principle procedure (2.5%). There were no flap failure events (Table 2).
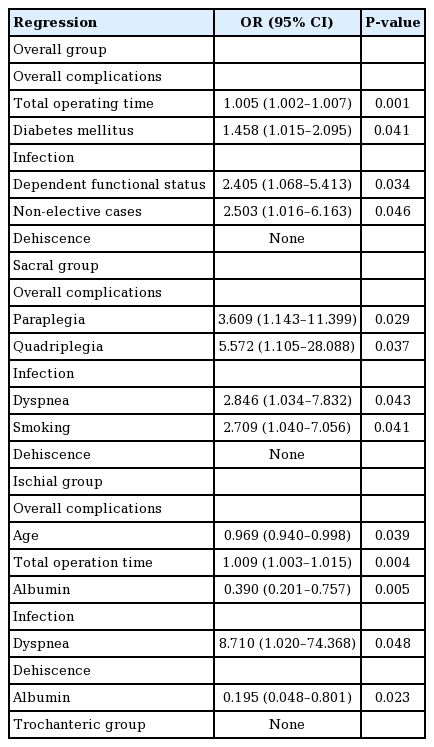
Independent risk factors for overall complications included total operating time (OR, 1.005; P=0.001) and DM (OR, 1.458; P=0.041). Partial or total dependency at baseline and emergency cases were risk factors for infection (OR, 2.405; P=0.034 and OR, 2.503; P=0.046, respectively). There were no identifiable risk factors for wound dehiscence.
Subgroup analysis
Intergroup comparison showed that the sacral decubitus ulcer group had the poorest baseline functional status. Overall, this group was the oldest (62 years vs. 51 years vs. 60 years), with the lowest albumin levels (2.5 g/dL vs. 2.9 g/dL vs. 2.8 g/dL), and highest incidence of comorbidities including DM, congestive heart failure, chronic obstructive pulmonary disease, recent myocardial infarction, HTN, history of cerebrovascular accident, history of chronic kidney disease on dialysis, and impaired sensorium. This group also had a higher incidence of coagulopathy (12.1% vs. 5.3% vs. 5.8%), total dependency (43.6% vs. 25.6% vs. 34.8%), ventilation dependency at baseline (5.2% vs. 0.6% vs. 1.4%), paraplegia (32.2% vs. 28% vs. 10.1%), and hemiplegia (4.1% vs. 1.6% vs. 1.4%). This group also had the highest incidence of emergency cases (8.5% vs. 1.9% vs. 1.4%) and class 3 and 4 contaminated wounds (91% vs. 86% vs. 84%). Lastly, the ischial group was noted to have the highest incidence of smoking (16.4% vs. 25.2% vs. 13%) and longest operating time (53 minutes vs. 95 minutes vs. 67 minutes).
The sacral decubitus group experienced the highest percentage of overall complications (27.7% vs. 21.5% vs. 26.1%, P=0.170). When examining individual complications, this group also had the highest percentage of bleeding requiring transfusion (12.3% vs. 6.2% vs. 10.1%, P=0.025), PE (0.5% vs. 0% vs. 0%, P=0.343), reoperation related to the principle procedure (1.9% vs. 1.6% vs. 0%, P=0.505), and infection (13.2% vs. 9.7% vs. 13%, P=0.339). It also had the longest LOS (16.25 days vs. 14.16 days vs. 10.38 days). Of note, only the incidence of bleeding requiring transfusion and of septic shock reached statistically significance. The highest incidence of dehiscence was noted in the ischial decubitus ulcer group (1.4% vs. 3.4% vs. 2.9%, P=0.203); however, this difference was not statistically significant. Incidence of DVT (0.8% vs. 1.2% vs. 1.4%, P=0.817) and readmission (2.5% vs. 2.2% vs. 4.3%, P=0.578) were highest in the trochanteric group, which again, was not statistically significant (Table 2).
Regression analysis for the sacral ulcer group revealed paraplegia (OR, 3.609; P=0.029) and quadriplegia (OR, 5.572; P= 0.037) as independent risk factors for overall complications. Independent risk factors for infection were preoperatively reported dyspnea (OR, 2.846; P=0.043) and history of smoking (OR, 2.709; P=0.041). There were no identifiable risk factors for dehiscence (Table 3).
In the ischial ulcer group, younger age (OR, 0.969; P=0.039), total operation time (OR, 1.009; P=0.004), and low preoperative albumin (OR, 0.390, P=0.005) were independent risk factors for overall complications. History of self-reported dyspnea preoperatively was the only risk factor for infection (OR, 8.710; P=0.048) and low preoperative albumin was the only risk factor for wound dehiscence (OR, 0.195; P=0.023). There were no identifiable risk factors for complications in the trochanteric ulcer group (Table 3).
DISCUSSION
Flap closure has become the mainstay surgical intervention for pressure ulcer reconstruction. However, the perioperative outcomes are less well described in the literature. In our study, we found that despite poor baseline physiological function, patients who underwent flap coverage for pressure ulcers experienced acceptable postoperative complications. Location of ulcer did not predict prevalence of complications. Instead, baseline patient characteristics correlated greatly with outcomes, with the sacral ulcer patients having the poorest baseline function and correspondingly highest complications. Identified independent risk factors for adverse outcomes consisted of a range of poor baseline characteristics, including those such as functional status, dyspnea, and low albumin, and varied depending on pressure ulcer location.
The reported overall complication rate in our study, 24.9%, appears to be relatively low in comparison to those reported in other reports that studied flap coverage for pressure ulcers. Two large retrospective studies by Keys et al. [7] and Bamba et al. [12] noted overall complication rates of 73% and 58.7%, respectively. The discrepancy between these two studies, as well as with ours, is most likely a result of differing follow-up periods, with longer term follow-up likely to reveal higher complication rates, and shorter-term follow-up, such as the 30 days in ACS-NSQIP, likely to reveal lower complication rates. When compared to a previous ACS-NSQIP study on pressure ulcer surgical treatment, we found that the rates were much more comparable, with Lim et al. [13] reporting a range from 20.6% to 28.9%. The variation between their study and ours likely stems from the fact that they incorporated a general range of ulcer management procedures, whereas we included solely flap coverage. In this instance, given that flap closure is technically more complex and used to close larger wounds, a higher incidence would be expected for complications such as wound dehiscence. It does appear, in this context, that flap reconstruction, regardless of ulcer site, has an acceptable overall complication rate, at least within a 30-day postoperative period.
Although there was no statistically significant difference between groups in terms of overall complications, there were some noticeable trends in individual complications. We found that patients who underwent coverage for the sacral ulcer experienced a higher incidence of septic shock and bleeding. Trochanteric pressure ulcer patients experienced a higher incidence of superficial SSI. This is in contrast to findings of multiple other studies stating that ischial ulcers are an independent risk factor for numerous complications [6-14]. The discrepancy might be explained by differences in duration of follow-up for other studies compared to ours. The higher rate of complications experienced after ischial pressure ulcer closure has been attributed to higher pressure at the ischial bony prominences, compared to other regions, in the sitting position [20]. However, within the 30-day time window of this study, perhaps there is inadequate time for certain complications to manifest.
Moreover, patient characteristics differences between sacral, ischial, and trochanteric pressure ulcer patients who underwent reconstruction may further explain the variation in ulcer site-specific complication rates. In our study, we found that patients who underwent reconstruction for sacral ulcers were significantly more diabetic, hypertensive, paraplegic, ventilation dependency, or required an operation in as an emergency. A significantly greater proportion of them also had lower albumin levels, more impaired sensorium, contaminated wound, ASA class 3 and 4, congestive heart failure, cerebrovascular accident, dialysis, or bleeding disorder. These factors have been recognized as risk factors for complications following flap coverage for ulcers [6-14,21,22]. Moreover, the higher incidence of specific comorbidities such as bleeding disorders are consistent with higher rates of bleeding, respectively. It therefore seems likely that the higher incidence of complications, notably septic shock and bleeding, in sacral pressure ulcer patients is a result of patients’ greater comorbidities.
The independent risk factors for overall complications in our total patient cohort were a longer operation time and diabetes, which is consistent with both the plastic surgery literature as well as studies from other surgical fields [21,22]. Diabetes has been recognized as a risk factor for complications ranging from infection to wound dehiscence [12,21,22]. Moreover, in previous pressure ulcer studies, pressure ulcer incidence has been notably higher in diabetic patients, as well as infection and recurrence when flap coverage is performed [21-23]. A longer operation time may be indicative of the complexity and size of the pressure ulcer and therefore, the extent of flap reconstruction, which may explain the higher complication rates.
Dependent functional status, both partial and complete dependency, was identified as an independent risk factor for infection. These patients might be less mobile, and hence less likely, or able to adhere to postoperative care instructions including frequent turning, pressure off loading, dressing changes, and hygiene requirements. Such conditions might contribute to complications such as wound infection. Non-elective cases were also recognized as a risk factor for infection. Understandably, patients who required urgent intervention may tend to have a more serious preoperative wound and systemic infection. As such, these patients are more likely to develop infection postoperatively.
In subgroup analysis of flap coverage by ulcer site, we found that paraplegia and quadriplegia were risk factors for overall complications in sacral ulcer patients. This is in concordance with the literature, noting that these comorbidities are risk factors for both pressure occurrence and complications [3,9]. We speculate that the patients who are otherwise physically limited may inherently have a poor baseline, which can contribute to a worse outcome profile. In addition, the inability to mobilize may contribute to increased pressure on the flap, leading to tissue ischemia, and ultimately, poorer outcomes. On the other hand, dyspnea and smoking were risk factors for infection. Smoking has been a recognized universal risk factor for numerous complications including infection in plastic surgery [24], as well as in a multitude of other disciplines. Dyspnea, on the other hand, may be explained by poor baseline functional status of these patients. Furthermore, in the event of dyspnea related to poor oxygenation, this may also affect wound healing, and predispose the patient to infection.
For patients with ischial ulcers, the identified independent risk factors for overall complications consist of young age, total operation time, and low albumin. Young age and total operation time as risk factors are well supported in prior studies on pressure ulcer management, regardless of follow-up time [6-14]. The argument is that younger patients may receive more complex or extensive reconstructive options, which are more prone to complications, and operation time may also be indicative of the complexity of the operation. Low albumin has been noted as an indicator of a patient’s overall medical fitness, in the context of malnutrition. Contrary to a previous study that found low albumin not being associated with worse 30-day outcomes in pressure ulcer management [13], our findings show it as a risk factor for overall complications and specifically, wound dehiscence. This difference in findings may be related to the nonspecific nature of the marker, our patient cohort consisting of only flap reconstruction, or variability in methodology. Dyspnea was noted to be an independent risk factor for infection, which could be explained as previously mentioned by both its role as a marker of patient baseline status or potentially related to tissue oxygenation.
We acknowledge the limitations of our study. A retrospective analysis of the ACS-NSQIP always has the potential error for human errors, both with coding and data entry, as well as the individual interpretations by researchers. Furthermore, another limitation is the 30-day follow-up period, which may not be sufficient for optimal capturing of all complications. This is particularly important to recognize for pressure ulcers, considering that one of the major outcomes of interest, ulcer recurrence, may take up to 15–22 months to occur according to studies [10,23,25]. The ACS-NSQIP database also has built-in variables for analysis, which limit the scope of our analysis. We were unable to evaluate size or depth of defect, number of ulcer recurrences, aspects of postoperative management such as patient positioning or time to ambulation, and surgical interventions performed prior to flap reconstruction.
Despite these factors, our study is the largest national study, to the best of our knowledge, evaluating perioperative outcomes of flap coverage for pressure ulcers. Sacral pressure ulcer patients who underwent flap reconstruction appear to have the greatest comorbidities and complication rates. Identified independent risk factors for adverse outcomes in pressure ulcer flap coverage patients consist of poor baseline patient characteristics, such as functional status, dyspnea, and low albumin. Recognition of these risk factors to identify high-risk patients may aid in optimization of outcomes and patient safety.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
This study is exempt from institutional review board (IRB) approval, as the ACS-NSQIP participant-use data files contain no protected health information.
Author contribution
Bao Ngoc N. Tran: collected the data; analyzed and interpreted the data; wrote the manuscript. Austin D. Chen: collected the data; provided critical revisions that are important for the intellectual content. Parisa Kamali: collected the data; provided critical revisions that are important for the intellectual content. Dhruv Singhal: provided critical revisions that are important for the intellectual content. Bernard T. Lee: analyzed and interpreted the data; provided critical revisions that are important for the intellectual content. Eugene Y. Fukudome: analyzed and interpreted the data; provided critical revisions that are important for the intellectual content. All authors conceived and designed the study and approved the final version of the manuscript.