Volar plate avulsion fracture alone or concomitant with collateral ligament rupture of the proximal interphalangeal joint: A comparison of surgical outcomes
Article information
Abstract
Background
Volar plate avulsion fracture of the proximal interphalangeal (PIP) joint is one of the most common hand injuries. In this study, we divided patients into two groups: patients with pure volar plate avulsion fracture, and patients with volar plate avulsion fracture concomitant with collateral ligament rupture. The purpose of this study was to compare long-term surgical outcomes between the two groups. As a secondary measure, the Mitek bone anchoring and polydioxanone (PDS) bone suturing techniques were compared.
Methods
A single-institutional retrospective review of the surgical treatment of volar plate avulsion fracture was performed. The cases were divided into those with pure volar plate avulsion fracture (group A, n=15) and those with volar plate avulsion fracture concomitant with collateral ligament rupture (group B, n=15). Both groups underwent volar plate reattachment using Mitek bone anchoring or PDS bone suturing followed by 2 weeks of immobilization in a dorsal protective splint.
Results
The average range of motion of the PIP joint and extension lag were significantly more favorable in group A (P<0.05). Differences in age; follow-up period; flexion function; visual analog scale scores; disabilities of the arm, shoulder, and hand scores; and the grip strength ratio between the two groups were non-significant. No significant differences were found in the surgical outcomes of Mitek bone anchoring and PDS bone suturing in group A.
Conclusions
Overall, the surgical outcomes of volar plate reattachment were successful irrespective of whether the collateral ligaments were torn. However, greater extension lag was observed in cases of collateral ligament injury.
INTRODUCTION
Volar plate avulsion fracture of the proximal interphalangeal (PIP) joint is one of the most common hand injuries resulting from hyperextension or rotatory force of the PIP joint [1]. Treatment goals include recovering PIP joint stability and achieving a normal range of motion (ROM). If untreated or inadequately treated, flexion contracture, recurrent subluxations, swan-neck deformity, and traumatic arthritis may occur [2].
Many comparative studies of factors affecting the functional outcomes of volar plate avulsion fracture have been conducted. In those studies, researchers compared, along with several other relevant variables, conservative and surgical treatment [3]; surgical outcomes of acute (<4 weeks) versus chronic (>4 weeks) fractures [4]; and bone fragment excision and bone fragment fixation [5]. In our study, we divided patients into two groups: those with pure volar plate avulsion fracture (group A) and those with volar plate avulsion fracture with collateral ligament rupture (group B). No study has yet investigated the effect of collateral ligament injuries on volar plate avulsion fracture. Additionally, whether one method of bone anchoring is superior to the other has not yet been explored.
Hence, the purpose of this study was 2-fold: (1) to statistically compare the surgical outcomes of the two groups and (2) to investigate differences between the Mitek (DePuy Mitek, Inc., Raynham, MA, USA) bone anchoring and polydioxanone (PDS; Ethicon, San Angelo, TX, USA) bone suturing techniques within the pure volar plate avulsion fracture group.
METHODS
This retrospective study was approved by our hospital’s Ethics Review Board (IRB no. KIRB-2018-N-001), and all patients provided informed consent for undergoing the procedures. From July 2009 to August 2016, we studied 30 patients who underwent surgical treatment at Gwangmyeong Sungae General Hospital for volar plate avulsion fracture. Only index, middle, ring, and little finger PIP joint injuries were considered. Of the patients, 15 had volar plate avulsion fracture without collateral ligament rupture (group A), and 15 had volar plate avulsion fracture concomitant with collateral ligament rupture (group B). In both groups, volar plate reattachment was performed using Mitek bone anchoring or PDS bone suturing.
The follow-up examinations included ROM; grip strength (assessed with the Jamar hand dynamometer; Patterson Medical, Bolingbrook, IL, USA) [6]; postoperative complications; visual analog scale (VAS) scores; disabilities of the arm, shoulder, and hand (DASH) scores; patient satisfaction; and radiographic status.
Inclusion criteria
The operative indications were an acute unstable fracture within 4 weeks of trauma, an avulsion fracture involving more than 30% of the joint surface, a bone fragment rotated by more than 90°, and the presence of dorsal subluxation.
Exclusion criteria
Cases of stable fractures, thumb injuries, multiple-finger injuries, open-wound injuries, and loss to follow-up within 1 year were excluded from the study.
Surgical technique
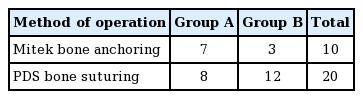
The procedure can be performed under regional or general anesthesia. We designed a Brunner or midlateral volar incision from the palmar digital crease to the distal interphalangeal flexion crease and elevated a skin flap. The lateral neurovascular structures were freed so that they were not under tension when the joint was exposed. The flexor sheath was incised between the A2 and A4 pulleys and the flexor tendons were retracted using a hook retractor. The volar plate, still attached to the fragments of the middle phalanx, was identified. Bone fragments were either reattached to the base of the middle phalanx together with the volar plate (24/30) or sharply excised from the volar plate (6/30) when the bone fragment was too small to reduce or hinder volar plate reattachment. Occasionally, when volar plate mobility was insufficient to advance to the base of the middle phalanx, the accessory collateral ligaments were released from the volar plate to maximize its mobility. In both groups, we either used a Mitek bone anchor (10/30) or PDS bone sutures (20/ 30) to reattach the volar plate to the base of the middle phalanx (Table 1). The choice of surgical method was determined by the preference of the surgeon.
Volar plate reattachment using Mitek bone anchoring
We predrilled a 1.3-mm hole in the center of the middle phalanx base and inserted the Mitek bone anchor into the hole at 45° to prevent the anchor from penetrating the cortex. Two strands of 4-0 Ethibond braided polyester sutures were applied to the lateral margins of the volar plate using two horizontal mattress sutures in order to preserve the width of the volar plate. To consolidate the repair, additional sutures were applied to the surrounding tissues, such as the periosteum (Fig. 1).
Volar plate reattachment using PDS bone suturing
Two small drill holes were made using a 0.9-mm Kirschner wire in both lateral-most portions of the trough in the middle phalanx base. A 23-gauge needle was passed through each drill hole to guide the suture needle. The 4-0 PDS was passed through each drill hole to suture both lateral margins of the volar plate using the figure-of-eight method. Additional sutures were applied to the surrounding tissues using the same method as Mitek bone anchoring (Fig. 2).
Polydioxanone bone suturing
(A) Two small drill holes were made using a 0.9-mm Kirschner wire in both lateral-most portions of the trough in the middle phalanx base. (B) The 4-0 polydioxanone (PDS) was passed through each drill hole to suture both lateral margins of the volar plate.
In group A, the volar plate and some degree of accessory collateral ligaments were ruptured but both proper collateral ligaments were intact; therefore, we repaired the volar plate alone. However, in group B, we observed concomitant volar plate rupture and complete rupture of the radial proper collateral ligament. Therefore, we repaired both the volar plate and the radial proper collateral ligament. Radial proper collateral ligament rupture was observed at the proximal attachment site. We carefully inspected the remnant of the radial proper collateral ligament on the condyle of the proximal phalanx to decide on the repair method. In six cases, the remnant of the collateral ligament was sufficient for direct suturing (6/15). However, in nine cases, the remnant was insufficient; therefore, we used Mitek bone anchoring (4/15) or PDS bone suturing (5/15) using the same technique as for volar plate repair. When the PIP joint was not sufficiently stable after volar plate reattachment, a Kirschner wire was placed at the PIP joint temporarily, to maintain joint stability, and was removed before the third week (5/30). The flexor sheath was repaired and the skin was closed. After assessing PIP joint stability and the perfusion of the finger, a dorsal protective splint was applied. Active motion was initiated at 2 weeks post-surgery with buddy taping of the involved finger and an adjacent finger, and full active and passive motion was encouraged at 4 weeks post-surgery.
Statistical analysis
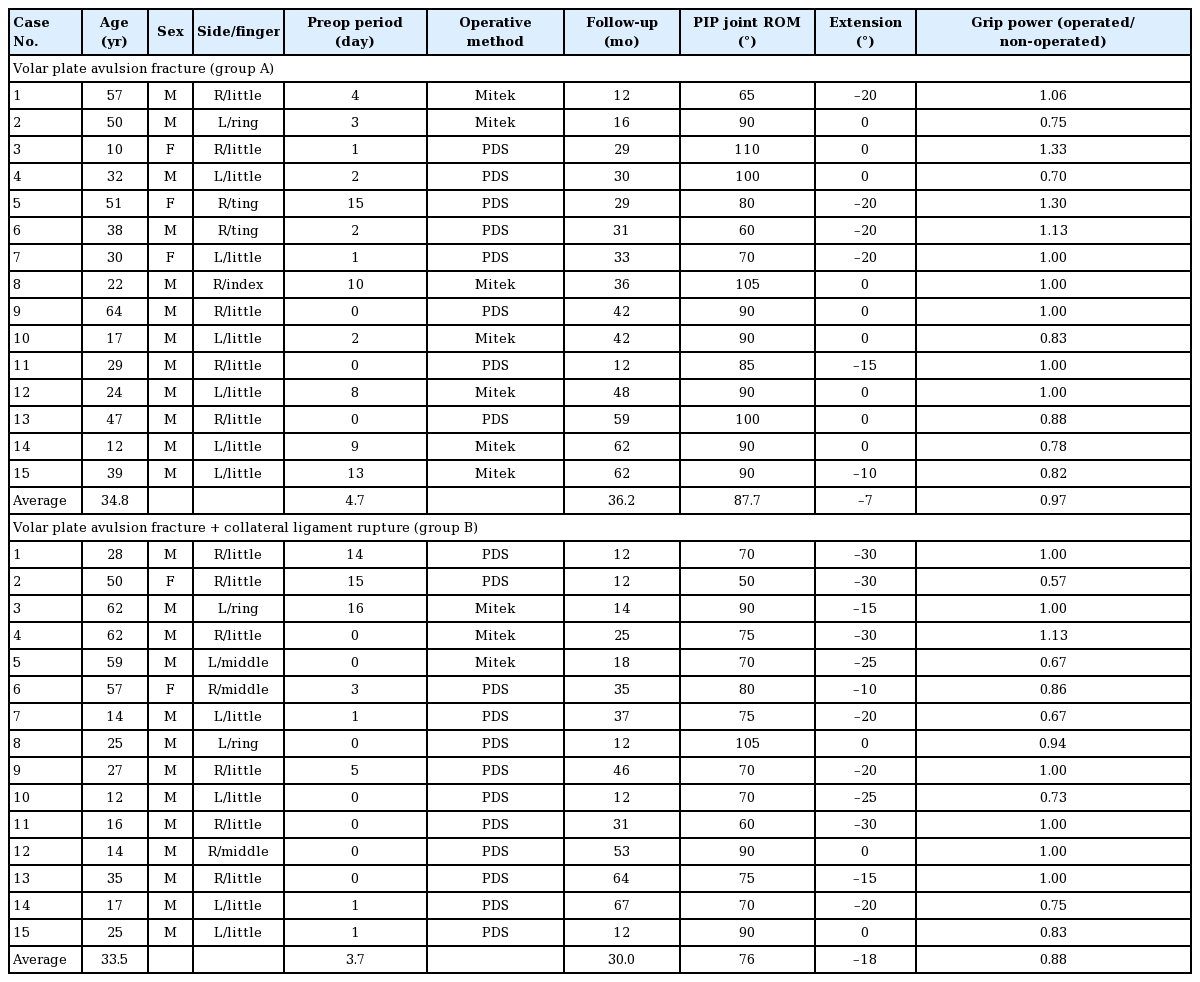
Patient age, follow-up period, ROM, extension lag, flexion function, the grip strength ratio of the injured to the uninjured hand, VAS scores, and DASH scores were compared between the two groups (Table 2). As a secondary measure, we also compared surgical outcomes between Mitek bone anchoring and PDS bone suturing in group A. The statistical analysis was performed with SPSS version 25.0 (IBM Corp., Armonk, NY, USA) using the Student t-test and the Mann-Whitney U test. P-values less than 0.05 were considered to indicate statistical significance.
RESULTS
Thirty patients (25 males, 5 females; 30 fingers) were evaluated during the follow-up. The average age of the patients at the time of surgery was 34.1 years (range, 10–62 years). Of the 30 fingers that were treated (1 index finger, 3 middle fingers, 5 ring fingers, and 21 little fingers), 14 were on the left hand and 16 were on the right hand. The most common causes of hand injury were slips (10 fingers) and the impact of a sports ball (10 fingers). The average interval between the injury and surgery was 4.2 days (range, 0–16 days), with surgery performed within 10 days in most cases (24 cases, 80.0%). The average follow-up interval was 33.1 months (range, 12–67 months).
The average PIP joint ROM was 87.7° and 76° in group A and B, respectively, and this difference was statistically significant (P=0.036). Flexion function was reasonably satisfactory in both groups (94.7° in group A and 94° in group B), with no significant difference (P=0.931). However, the differences in average extension lag were larger. Group A recorded an average extension lag of 7° (9 fingers had full extension), and group B recorded 18° (3 fingers had full extension), which was a significant difference (P=0.009). The average grip strength of the injured finger compared to that of the contralateral finger was 97% for group A and 88% for group B, but this difference was not statistically significant (P=0.519) (Fig. 3).
Comparison of outcomes in two groups
The average proximal interphalangeal joint range of motion (ROM) and extension lag were significantly more favorable in group A (P=0.036 and P=0.009, respectively, using the Mann-Whitney U test). Left axis: ROM, flexion, grip power; right axis: extension.
The average age in both groups was 34.8 and 33.5 years, respectively (P=0.956). Overall, the PIP joint ROM appeared less favorable for older patients; however, because of the small sample size, this difference was not statistically significant. Group A had a longer preoperative period (4.7 days) than group B (3.7 days), but this was not statistically significant (P=0.545). The average follow-up period for groups A and B was 36.2 and 30.0 months, respectively, with no significant difference (P=0.337). The VAS and DASH scores likewise did not show statistically significant differences between the two groups.
Finally, no significant differences were found in the surgical outcomes of Mitek bone anchoring and PDS bone suturing in group A (Fig. 4).
Mitek anchoring and PDS suturing outcomes comparison
No significant differences were found between the two methods in group A (Mann-Whitney U test). Left axis: ROM, flexion, grip power; right axis: extension. PDS, polydioxanone; ROM, range of motion.
Complications
No patients complained of infection, postoperative pain, joint instability, sensory problems, or angular deformity. No clinical evidence of residual joint instability was identified in any patients.
Case 1 (group A)
A 32-year-old man sustained dorsal dislocation of the PIP joint in the left little finger while playing basketball. Manual reduction under digital block was performed at the emergency room on the day of the trauma, and surgery was performed 2 days later. During surgery, complete volar plate rupture with avulsion fracture was found. The bone fragments were sharply excised and the volar plate was sutured to the base of the middle phalanx using 4-0 PDS. At the 30-month follow-up, the patient had full, painless motion at the PIP joint (0°–100° active motion) and symmetrical grip strength. Radiology films showed no degenerative changes (Fig. 5).
Case 1 (group A)
(A) Complete rupture of the volar plate with avulsion fracture was found and reattached using polydioxanone (PDS) bone suturing. (B, C) At the 30-month follow-up, the proximal interphalangeal (PIP) joint range of motion was from 0° to 100°. (D) Preoperative radiological findings showing volar plate avulsion fracture of the PIP joint rotated by more than 90°. (E) Postoperative radiological findings. The bone fragments were excised and the volar plate was sutured to the middle phalanx base using 4-0 PDS.
Case 2 (group B)
A 59-year-old man slipped and sustained a lateral rotatory dislocation of the PIP joint in the left middle finger. Radiology films showed a dorso-ulnar dislocation of the PIP joint with a displaced volar plate avulsion fracture of the middle phalanx. Physical examination showed PIP joint hyperextension instability and more than 30° deformity on the varus stress test. Emergency surgery was performed on the day of trauma. During surgery, complete rupture of the volar plate and radial collateral ligament was observed. The volar plate was reattached to the middle phalanx base using Mitek bone anchoring, and the radial collateral ligament was sutured to the proximal phalanx head using 4-0 PDS. At 18 months of follow-up, the patient was found to have full flexion with slight extension lag (25°–95° active motion) in the PIP joint. No other postoperative complications were observed and the patient was satisfied with the outcomes (Fig. 6).
Case 2 (group B)
(A) The volar plate was reattached to the middle phalanx base using Mitek bone anchoring. (B) The radial collateral ligament was sutured to the proximal phalanx head using 4-0 polydioxanone (PDS). (C) Schema of the volar plate and radial collateral ligament repair. (D) Preoperative radiology showing dorso-ulnar dislocation of the proximal interphalangeal joint with volar plate avulsion fracture. (E) Postoperative radiology. The fracture was reduced by the Mitek bone anchor.
DISCUSSION
The PIP joint is a synovial hinge joint (range, 0° to 100°–110°) surrounded by a box-like ligamentous complex, secured laterally by collateral ligaments and volarly by the volar plate [7]. The volar plate originates from the periosteum of the proximal phalanx head, known as the checkrein ligaments, inserts into the volar periosteum of the middle phalanx base, and is suspended laterally by the accessory collateral ligaments [8]. The proper collateral ligaments arise from each side of a concave fossa of the proximal phalanx head and extend obliquely and distally to their insertions in the middle phalanx base. The volar plate is an important structure for maintaining anterior and posterior stability, and the collateral ligament is an important structure that maintains lateral stability.
Normally, some degree of hyperextension is possible, but this varies considerably across individuals. For dislocation of the PIP joint, at least two planes of the ligament complex must be disrupted [1]. Typically, the volar plate avulses distally because the proximal part is firmly attached by the checkrein ligament to the proximal phalanx [9]. However, the collateral ligament ruptures at the weakest point of its proximal attachment. As the rupture of these ligaments usually occurs at their attachment sites on the bone, anchoring techniques are conventionally required (Fig. 6C).
Acute dorsal PIP fracture/dislocation (as in group A) results from PIP joint hyperextension combined with a longitudinal compression force, and it is most frequently caused by a ball forcefully hitting the fingertip. The volar plate, as well as the accessory collateral ligaments to some degree, might be ruptured by such a trauma vector, but it is not necessary to repair the accessory collateral ligaments [1]. However, lateral rotatory fracture/dislocation (as in group B) is caused by a rotatory force on the PIP joint. A typical mechanism of injury involves catching a gloved digit in a spinning drill or manually twisting a digit. More than 20° deformity of extension on gentle static lateral testing indicates complete collateral ligament disruption and injury to at least 1 other secondary stabilizer [10]. Interestingly, in our study (group B), collateral ligament rupture was observed only on the radial side. If we consider the functional anatomy of the hand, it can be assumed that the direction of the trauma vector is towards the dorso-ulnar side; hence, the radial collateral ligament tends to be ruptured more commonly than the ulnar collateral ligament. For the same reason, the little finger is the most commonly affected finger.
In 1980, Eaton and Malerich [11] described successful resurfacing results for classic volar plate arthroplasty in 24 patients. They used a wire suture spiraled along the lateral margins of the volar plate as the pull-out suture. However, this method had several significant disadvantages, including wire laxity, the risk of middle phalanx infection through the opening to the bone, necrosis or pressure sores of the dorsal skin, as well as patient discomfort with the presence of the external wire pressing against the skin [12]. Our technique involved using Mitek bone anchoring and PDS bone suturing, which are superior to the pull-out-wire technique for wound care and rehabilitation. Previous studies have suggested that releasing the volar plate from the bilateral accessory collateral ligaments is necessary to increase the mobility of the reattachment and to improve the final PIP joint ROM [11,13,14]. However, because all our cases were acute, most of the volar plate advancements were possible without removing the accessory ligaments.
Because the most common sequela of ligament injuries of the PIP joint is stiffness, not instability, the surgical trauma of volar plate repair may have an adverse effect on the final ROM of the joint [1]. In 2013, Werlinrud et al. [3] reported that a majority of volar plate avulsion fractures could be managed successfully with conservative treatment. However, previous reports of successful conservative treatment did not consider the risk of joint stiffness from prolonged immobilization [15]. Moreover, if several weeks of conservative treatment fail, excessive scarring of the volar plate and overall extensor tendon adhesion secondary to lengthy preoperative immobilization can contribute to extension lag in patients undergoing late surgery. In our cases, early and strong repair of the volar plate and collateral ligament provided sufficient mechanical stability for quicker postoperative rehabilitation and functional recovery. Although we were not able to conduct a comparative study of conservative and surgical treatment because of the lack of a control group, surgical outcomes such as flexion, grip power, and ROM showed satisfactory recovery of function.
This study has several limitations. First, since the sample size was small, the significance of our statistical analysis was limited. Second, it was a retrospective comparative study, not a randomized case-control study; thus, our results may have been affected by bias. Therefore, future prospective randomized studies with larger sample sizes are required. In addition, a comparison between conservative and surgical treatment might provide novel insights into outcomes.
Volar plate avulsion fractures are the most common and under-treated joint injuries of the hand. The recommended treatment varies widely. To achieve optimal results in volar plate reattachment, certain details must be understood. In our study, regardless of whether the collateral ligaments were torn, the surgical outcomes of early volar plate reattachment using Mitek bone anchoring and PDS bone suturing were successful. However, greater extension lag was observed in cases of collateral ligament injury.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Sungae General Hospital (IRB No. KIRB-2018-N-001) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.