Internal jugular phlebectasia (IJP) is defined as a fusiform dilatation of the internal jugular vein without tortuosity [1]. IJP is diagnosed on physical examination and Doppler ultrasonography. However, it rarely presents symptoms or complications. It is commonly recommended that regular monitoring of its clinical course be performed, and sometimes surgery is performed for cosmetic purposes [2-5]. We report a case of a 40-year-old woman with facial trauma with a review of the literature.
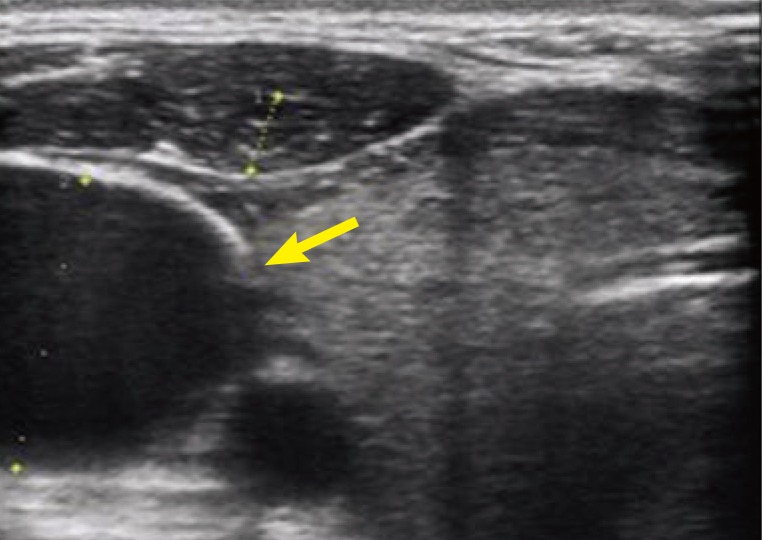
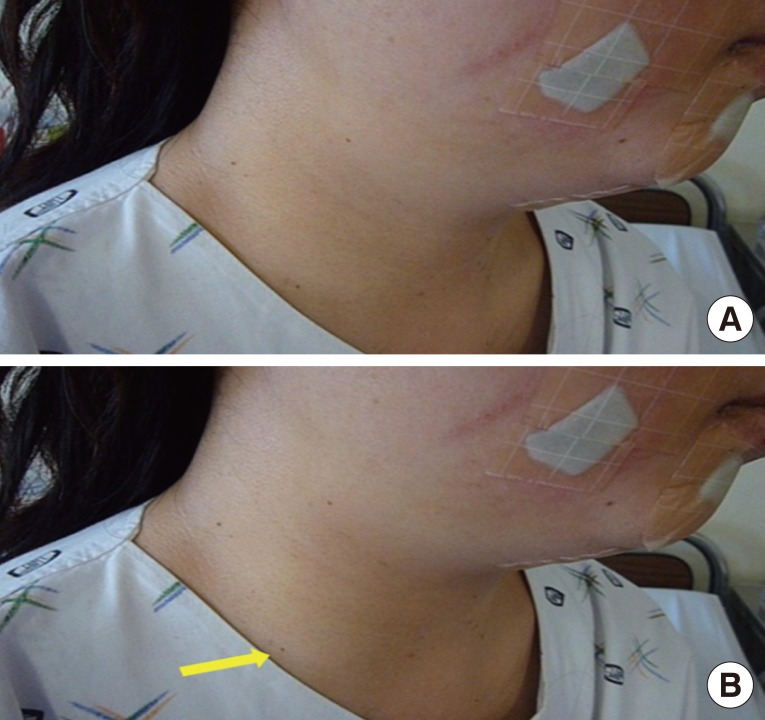
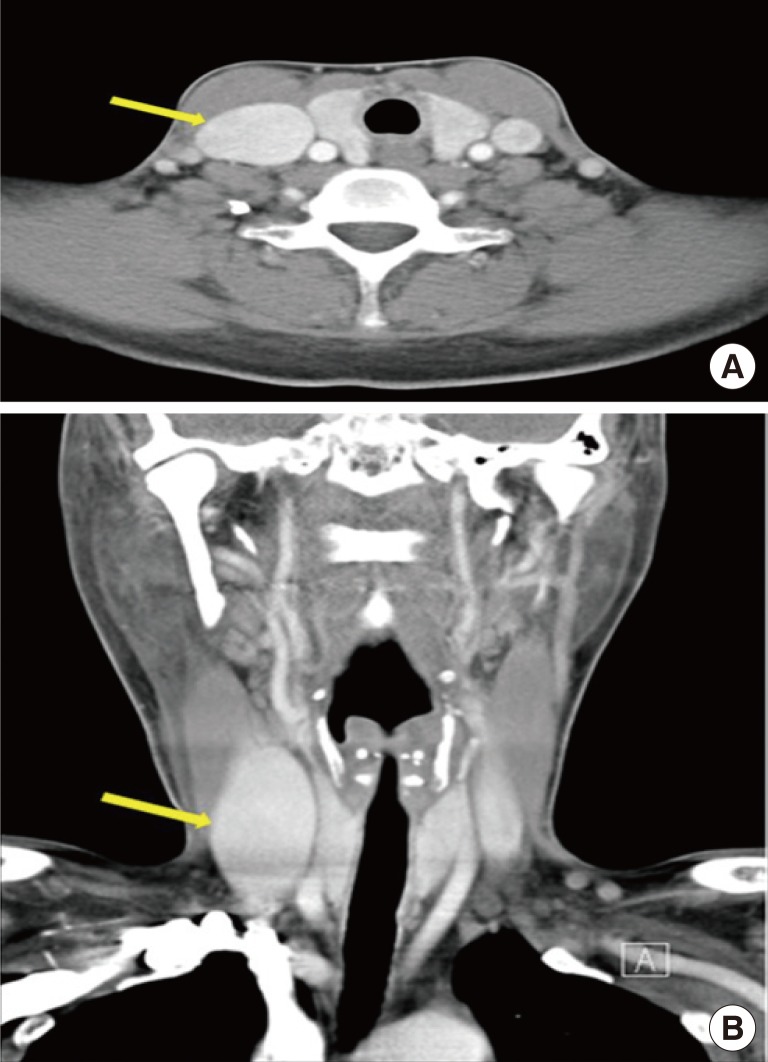
A 40-year-old woman visited the Department of Emergency Medicine with chief complaints of facial laceration and complex fracture of the right zygomatic bone after a motorcycle traffic accident. The patient had no comorbidities other than iron deficiency anemia that was being controlled with an oral iron supplement. Because the patient presented right neck swelling, Doppler ultrasonography was performed to rule out a diagnosis of delayed rupture of the cervical vessels. However, it revealed no definite abnormalities other than the dilatation of the right internal jugular vein (Fig. 1). After open reduction and internal fixation of the zygomatic fracture, a physical examination was performed. This showed an enlargement of the neck swelling during a Valsalva maneuver. We tried to find any causative structural lesions such as a cervical or laryngeal mass, but computed tomography (CT) scans showed no definite structural abnormalities (Figs. 2,3). The patient had no symptoms and refused surgery for follow-up, the patient presented with no complications.
IJP is a rare condition and its epidemiologic features have not been well documented. In recent years, its incidence has increased. This is attributable to an increased number of diagnoses of subclinical cases because of advancement of diagnostic imaging modalities and increased frequency of laryngeal and cervical surgery [1,2]. Two hypotheses have been proposed to explain the etiology of IJP: The first is the elevated pressure in the internal jugular vein and the second is the congenital defect of the venous wall. If there is a mediastinal or cervical mass, it could disturb the venous drainage or cause regurgitation of venous flow. This eventually leads to the increased hydrostatic pressure and dilatation of the vessel. Second, if there is a congenital defect of the venous wall, this could also cause IJP. Surgical specimens have shown a loss of elastic tissue, thinning of the venous wall, fibrosis, and a decrease or absence of the smooth muscle layer [1,2].
IJP can be diagnosed by flow in Doppler ultrasonography and dilation during the Valsalva maneuver. In addition, any causative structural lesions should be ruled out on CT scans [2]. Complications that occur in rare cases include progression, thrombosis, and Horner's syndrome. The chief complaint of patients is cosmetic concerns [1-4]. Clinical surveillance is usually recommended when there are no symptoms or complications. In these cases, however, surgery is a possible treatment option. Conventional surgical procedures consist of ligation of the internal jugular vein through a transcutaneous cervical approach or transaxillary approach [3,4]. Venoplasty or anastomosis after resection of the affected lesion has been performed successfully to preserve the physiologic blood flow of the cervical vessels, especially in bilateral cases [5]. In the current case, we decided to follow-up with the patient on a monthly basis, not only because there were no symptoms or complications, but also because the radiologic study revealed only the dilatation of the internal jugular vein without any causative structural lesions. In addition, the patient refused to undergo cosmetic surgery.
In evaluating patients with trauma who experience neck swelling, clinicians should consider making a differential diagnosis of various conditions from simple contusion to life-threatening ones including pseudoaneurysm or a delayed rupture of the cervical vessels. These life-threatening vessel injuries can be confirmed by angiography, which should be accompanied by emergency intervention or surgery. Although IJP is a rare condition, when making a differential diagnosis of neck swelling in patients with trauma, clinicians should refrain from unnecessary evaluations by performing a physical examination and routine radiography to conserve time and money. We experienced a rare case of IJP in a patient with trauma. Clinicians should be aware of IJP as a candidate condition of the differential diagnosis of neck swelling in trauma patients.