INTRODUCTION
Patients with a repaired cleft lip/palate often have diminished transverse and sagittal maxillary growth. The upper jaw is unable to keep up with the normal growth of the lower jaw, thus adversely affecting both the facial profile and dental occlusion. Approximately 21% of patients with clefts developed maxillary hypoplasia/retrusion requiring maxillary advancement [
1]. The LeFort I maxillary osteotomy is a frequently performed operation used to resolve abnormalities of the jaw relationship in these patients. Maxillary advancement can normalize dental occlusion and may result in improved articulation, that is, the shaping of the vocal tract using the lips, tongue, jaw, and velum for speech output [
2]. However, it may also alter the velopharyngeal relationship because movement of the maxilla results in movement of the posterior border of the hard palate with its soft palate attachment. Patients who already have velar deficiencies would have a higher risk for developing velopharyngeal insufficiency.
Nevertheless, the effect of maxillary advancement on the velopharyngeal mechanism remains controversial. Published articles have not shown robustness of data [
3-
6].
The aims of this study were to investigate the impact of maxillary advancement in patients with repaired cleft palate but without deterioration in velopharyngeal function before maxillary advancement.
METHODS
Subjects
This study focused on patients who underwent maxillary advancement for 6 years between 2005 and 2011. Twenty patients were diagnosed with maxillary retrusion, 18 patients underwent LeFort I osteotomy, and 2 underwent distraction osteogenesis. To avoid bias associated with the surgical method, we studied the 18 patients underwent LeFort I osteotomy between the ages of 11 to 20 years. Two of them had undergone pharyngeal flap for the correction of velopharyngeal inadequacy (VPI) before maxillary advancement surgery. One patient was excluded from our study due to evidence of impairment on the preoperative perceptual speech test.
To investigate the impact of maxillary advancement in patients with repaired cleft palate, we divided the patients into group A, with repaired cleft palate, and group B, without cleft palate.
Surgical technique
A single surgeon did the maxillary advancement on all patients. For LeFort I osteotomy patients, the osteotomy extended from the piriform aperture to the pterygoid plates above the apices of the teeth. Using dental cast and cephalometric X-ray analysis, the amount of advancement was planned to satisfy aesthetic demands while normalizing occlusion. Maxillary advancement up to 10 mm could be achieved by LeFort I osteotomy. In two patients that had needed more advancement than 10 mm, the facial profile could not be corrected by LeFort I osteotomy alone, and therefore they also underwent a sagittal split ramus osteotomy of the mandible.
Perceptual speech and resonance assessment
Speech assessments were performed preoperatively and at least 8 months postoperatively. The assessment evaluated nasal emission, articulation, and hypernasality by speech language pathologists. The examination was conducted twice at each preoperative and postoperative period by two different examiners. Nasal emission was evaluated by using a mirror. Each patient was asked to read a protocol that consisted of a list of single words designed by Ok-Ran Jung [
7] (
Table 1).
The scoring for nasal emission was as follows: 1 was no nasal emission and 0 was existence of nasal emission. We tested 10 words for nasal emission and the total score was 10.
The score of hypernaslity and articulation was as follows: 3 was normal or no change, 2 was hypernasality or speech distortion of slight to moderate degree that could be comprehensive, and 1 was severe hypernasality or severe speech disturbance that could not be comprehensive. Ten words were tested for hypernasality and the total score was 30. And 19 words were tested for articulation and the total score was 57.
Statistical analysis
Statistical analysis was performed by using the statistical package SPSS ver. 18.0 (IMB, Armonk, NY, USA). Wilcoxon signed rank test was used to determine if there were significant differences between the preoperative and postoperative outcomes in each group A and B. And Mann-Whitney U test was used to determine if there were significant differences in the change of score between groups A and B.
RESULTS
Group A involved 8 patients that had a repaired cleft palate and group B involved 2 patients that had a bilateral complete cleft lip without cleft palate, 1 patient that had hemifacial microsomia, and 6 patients that were free from cleft lip/palate or other craniofacial syndromes. All patients scored normally on the perceptual speech test before maxillary advancement.
No patient presented a change in nasal emission postoperatively. The mean nasal emission score was 8.65±0.42 in group A and 9.20±0.36 in group B.
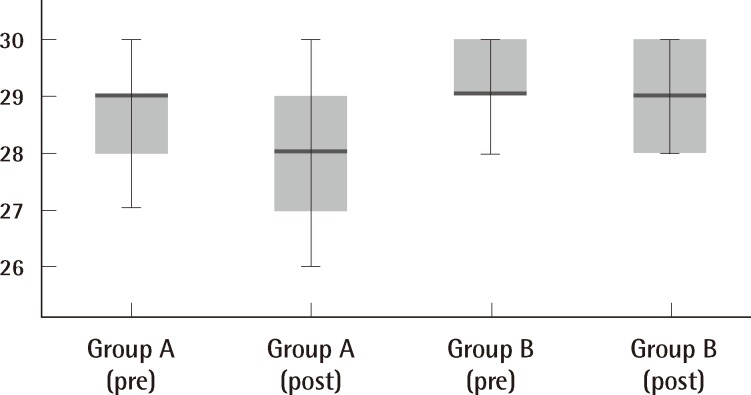
The median (interquartile range, IQR) of the hypernasality score of group A was 29 (28-29) preoperatively, and 28 (27-29) postoperatively. Wilcoxon signed rank test showed no significant differences between pre and postoperative scores in group A (P=0.062). The median (IQR) of the hypernasality score of group B was 29 (29-30) preoperatively and 29 (28-30) postoperatively. Wilcoxon signed rank test showed no significant differences between pre and postoperative scores in group B (P=0.109). And Mann-Whitney U test showed no significant difference between the changes in two groups (P=0.152) (
Fig. 1).
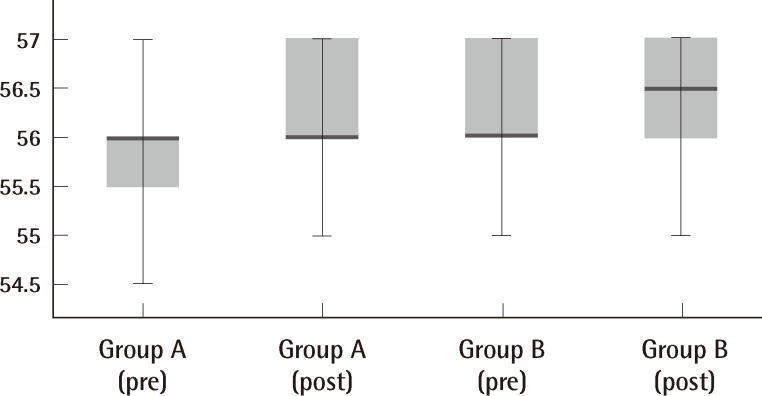
Preoperatively, The median (IQR) of the articulation score of group A was 56 (55.5 to 56): the mean postoperative score increased to 56 (56 to 57). Wilcoxon signed rank test showed no significant differences between pre and postoperative scores in group A (P=0.414). The median (IQR) of the articulation score of group B was 56 (56 to 57) preoperatively and 56.5 (56 to 57) postoperatively. Wilcoxon signed rank test showed no significant differences between pre and postoperative scores in group B (P=0.183). And Mann-Whitney U test showed no significant difference between the changes in two groups (P=0.499) (
Fig. 2).
DISCUSSION
In a study by Schwarz and Gruner [
8], 84% of VPI cases occurred after maxillary advancement in patients with cleft palates. Their research subjects, however, had hypernasality to some degree prior to LeFort I osteotomy.
Chanchareonsook et al. [
5] systematically reviewed 39 studies from the past 30 years. They classified the studies into three categories: those in which the velopharyngeal function worsened after maxillary advancement, regardless of the preoperative VPI status; those in which the velopharyngeal function worsened after maxillary advancement in patients with borderline velopharyngeal function preoperatively; and those in which there was no association between maxillary advancement and velopharyngeal function. They reported that although maxillary advancement had good outcomes for the facial appearance and occlusion in these studies, and had a positive impact on articulation, the patient undergoing it has the risk of deterioration in velopharyngeal function for speech.
Chua et al. [
9] reported that velopharyngeal function and maxillary advancement showed a negative correlation with each other. They stated, however, that even a small advancement such as 4 mm resulted in deterioration in the velopharyngeal function, and so implied that even small amount of maxillary advancement can have an absolute impact on velopharyngeal function.
According to McComb et al. [
10], citing David and Sader, a maxillary advancement of over 7 or 10 mm could have an adverse effect on the velopharyngeal function. At the same time, however, they also mentioned other studies that showed no correlation between maxillary advancement and velopharyngeal function.
Schendel et al. [
11] showed that cleft palate patients are more vulnerable to maxillary advancement than non-cleft palate patients. By comparing the structural adaptation of the soft palate in cleft palate and non-cleft palate patients, they found that a repaired cleft palate lacked the ability to adapt to changes in the pharyngeal depth after maxillary advancement. They suggested that palatal scarring interfered with soft palatal adaptation to the pharyngeal depth. Thus, they claimed that repaired cleft palate patients with short soft palates had an increased risk of VPI after maxillary advancement surgery.
Although patients with a repaired cleft palate have palatal scars, in our series we had no difficulty performing advancement, and could not verify any connection between postoperative speech outcome and a repaired cleft palate. In addition, we did not find deterioration in velopharyngeal function after maxillary advancement compared with non-cleft palate patients, even in the 1 patient who underwent pharyngeal flap surgery before maxillary advancement. The maxillary advancement could also reduce snoring after pharyngeal flap. As a repaired cleft palate patient has scars in the lips, nose, and palate, it is not easy to advance the maxilla more than 10 mm. With full mobilization, however, it is sufficient to advance the maxilla up to 10 mm. In patients who need more than 10 mm advancement, we prefer to perform sagittal split ramus osteotomy of the mandible with maxillary advancement. If the patient develops VPI, we can improve the speech by pharyngeal flap.
To prevent hypernasality, it is essential for the pharyngeal wall and soft palate to collaborate, and for the nasopharynx and oropharynx to be separated. If the maxilla is advanced too far for the velopharynx to close completely, VPI will develop. Therefore, the more advancement is performed, the greater the risk of deterioration in velopharyngeal function. Nevertheless, we believe that there is no need to hesitate in performing advancement in fear of development of VPI because the improvement of the facial morphology is more important for the patient than any slight deterioration in velopharyngeal function.
In this study, we used perceptual measurements to evaluate velopharyngeal function. We usually perform further anatomic and physiologic evaluation when the result of perceptual measurements is abnormal. Our subjects had normal speech preoperatively according to the perceptual assessment, so we had not collected other preoperative anatomic or physiologic data on our subjects. However, perceptual speech evaluation is the basis of speech assessment and is adequate for determining whether there is velopharyngeal dysfunction, the type (insufficiency, incompetence, or mislearning), and the approximate size of the opening [
12,
13]. Furthermore, Peterson-Falzone et al. [
14] claims that perceptual evaluation of hypernasality is the "single-most important assessment tool that the speech language pathologist will use in clinical practice" for evaluating the speech of individuals with cleft palate. Kim et al. [
15] reported that the perceptual ratings significantly correlated with the objective measures of sound spectrography.
However, Chanchareonsook et al. [
16] advocated using both perceptual speech measurement (such as articulation and nasality) and velopharyngeal status assessment. We are also collecting data using perceptual speech measurement, cephalometry, nasometry, videofluoroscopy, and nasendoscopy. A group of patients with repaired cleft palate whose velopharyngeal function worsened after maxillary advancement will be compared with a group of repaired cleft palate patients whose velopharyngeal function did not worsen, in order to determine the factors that are significantly related to the deterioration in the velopharyngeal function among various preoperatively measured values (e.g., soft palatal length, pharyngeal depth, pharyngeal wall mobility, etc.). With these efforts, it will be possible to perform maxillary advancement more safely in cleft palate patients.
The purpose of this study was to determine whether maxillary advancement has a greater influence on velopharyngeal function in patients with repaired cleft palate than non-cleft palate patients. The results showed that there is no significant correlation between a repaired cleft palate and velopharyngeal function. The patients with repaired cleft palate and without velopharyngeal dysfunction preoperatively did not have greater deterioration in velopharyngeal function after maxillary advancement than the non-cleft palate patients.
This study reports on speech outcomes after maxillary advancements of cleft cases compared with non-cleft cases. Suggestions for further study and for helping with case management were introduced as well. Our society has produced few studies on this topic. Therefore, the authors' results have advanced our knowledge to the benefit of our plastic and maxillofacial surgeons.
There are many important factors in studying orthognathic surgery, velopharyngeal function, and their relationships. Among them, adequate case study selection, defining cephalometric analysis for structural evaluation, and optimal evaluation of velopharyngeal function should be well designed to produce acceptable results.
Considering the complexity of oral and maxillofacial structures, orthognathic surgery is a complicated procedure. The nature of the skin and subcutaneous tissue, muscles, ligaments, and hard tissue resilience differ a little in each case. In addition, cleft cases are far different from non-cleft cases because of operative scars, structural asymmetry of hard and soft tissues, and growth deformity. Most cleft maxillary movement vectors are three dimensional, and that results in frequent misdiagnosis. Therefore, adequate case selection is the most important factor in orthognathic surgery study, especially in cleft cases. Cases involving simple jaw movement such as pure advancement, those with simple definitions such as unilateral cleft lip and palate, and those involving one surgeon make the best subjects of study [
1].
Delicate structural analysis can be made by defining cephalometric analysis because cephalometric analysis with a cephalogram has been evaluated for ninety years and many analytical methods and prediction mechanisms have been developed. However, mis-tracing as well as inter-observer and intra-observer biases can occur in assessing cephalograms. To reduce mis-tracing and biases, these studies would be better performed in conjunction with dental specialists such as orthodontists or oral surgeons. Two or more specialists trace the cephalograms and perform the trace at least twice with a time interval of at least one week. Special caution should be applied to cleft cases because of anatomical differences. For example, a posterior nasal spine is defined as the process formed by the united projecting ends of the posterior borders of the palatal process of the palatal bone. In cleft palate cases, both of the posterior borders of the palatal process make hardly unification. Therefore, a researcher should find that point using a pterygomaxillary fissure, which is the contour of the fissure projected onto the palatal plane. In addition, an A-point is widely used. An A-point is the point of greatest concavity on the anterior border of the maxilla. However, it is difficult to identify in cleft cases because of anterior nasal spine deviation and dentoalveolar abnormality. Therefore, a new A-point should be made for cleft cases. Follow-up cephalograms should be taken after at least a year to confirm the results [
2,
3].
Optimal evaluation of velopharyngeal function is essential for producing acceptable results. A recent review of speech outcomes recommends at least one instrumental measure such as naso-endoscopy, multiview videofluoroscopy, nasometry, pressure-flow analysis, and perceptional speech analysis. A follow-up of at least 6 months is essential [
4,
5].
In conclusion, stable and reproducible surgery, reliable cephalogram analysis after at least one year, and at least 6 months follow-up using multiple measurements of speech outcomes can produce acceptable results for orthognathic-velopharyngeal function research.