INTRODUCTION
Congenital melanocytic nevi (CMN) of the face are common malformations that are very problematic for patients. The optimal management of CMN has been a longstanding surgical challenge, due to the need for a complete excision of the lesion and the problem of aesthetic disfigurement from scarring [1-4].
The traditional method for nevus excision is elliptical design. This pattern allows primary closure without dog ear formation. Usually, the recommended length-to-width ratio is between 3.0 and 4.5 [5,6], but this results in a longer scar than the primary lesion. The surgeon usually sacrifices a significant amount of normal skin, as attempts to excise less skin result in dog ear formation.
To minimize tension for wound approximation, wider subcutaneous undermining is required. After wound closure, however, the distortion of important normal facial structure is possible. Planning the width of the excision is not easy, because the tissue tension after wider undermining and the distortion of normal structures are usually not equal to those predicted preoperatively. Unfortunately, changing the plan to serial excision because of excessive tension is generally inappropriate after the removal of a total lesion.
In this study, we carefully compared the outcomes of the predicted results of planned elliptical designs with those achieved after excision with our alternative technique using one side incision and multidirectional vector wound closure.
METHODS
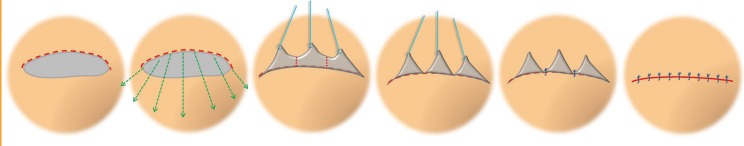
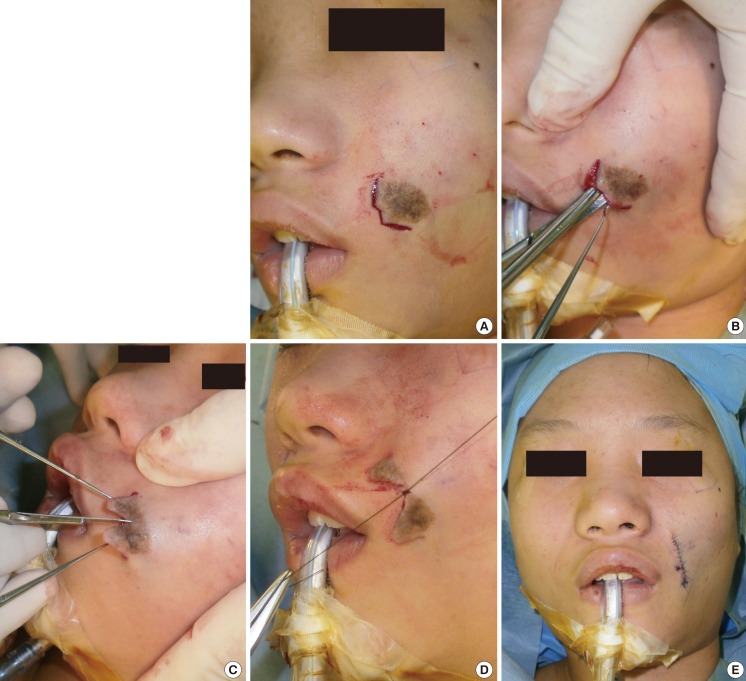
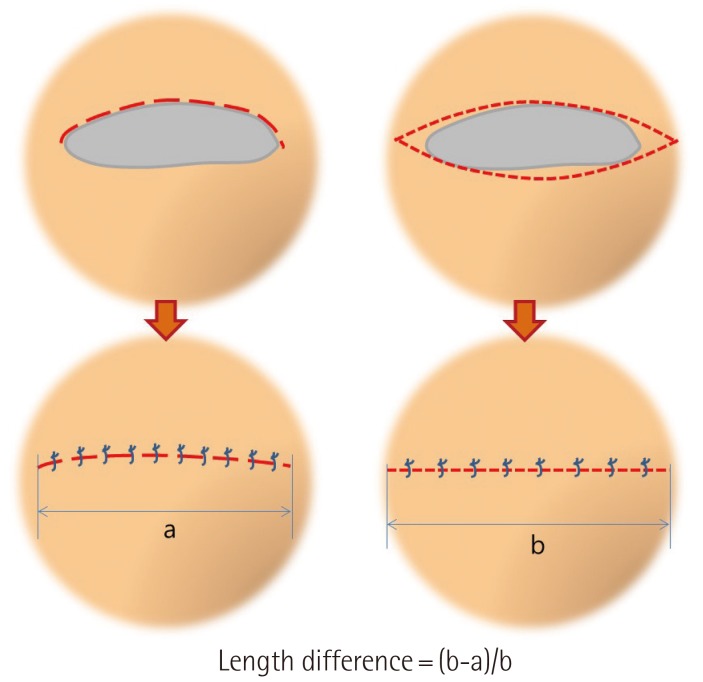
A total of 82 patients with CMN were treated with this technique in our institution during the period from 2000 to 2012. 34 were males, and 48 were females. Their age ranged from 6 months to 31 years. Each lesion was examined and an excision margin along the nevus border was drawn on the face. The potential scar length with an elliptical excision method was calculated as 3 times the planned excision width. In practice, we incised only one side margin of the nevus-the side which was closer to a critical structure such as an eyebrow, nose, eyelid, or lip (Figs. 1, 2). After subcutaneous undermining beneath the lesion, extensive dissection of normal tissue was necessary for approximation following nevus removal. The direction of undermining should be in the opposite direction of critical structures to avoid the distortion of normal facial anatomy. Once adequate undermining was performed, the skin flap including the nevus was pulled over the normal skin with skin hooks. The optimal vectors of skin hook traction were not even because the factors that affect tension and dog-ear deformity-the elastic properties of skin, wound geometry, and surface contour-vary with the location. Ideal vectors are those that cause minimal dog-ear deformity and produce reasonable tension for wound approximation. After carefully deciding on the vectors of traction, the flap was divided in several pieces with slit incisions made by a scalpel at a right angle to the defect margin. If we predict excessive tension from the excision of the entire nevus, the plan should be changed to a partial excision for better postoperative results and slit incisions should be limited to a proper portion of the total width. Several key sutures were then placed at the apices of the notch, followed by the confirmation of normal structure distortions and dog-ear deformity. If a distortion of a facial subunit is definite, the flap to be removed should be designed to be smaller. Despite choosing an ideal vector to minimize dog-ear deformity, sometimes some minor dog-ear formation cannot be avoided. In such cases, mounds of excess skin were removed via a standard dog-ear correction technique. If the key sutures are placed with minimal distortion and unnoticeable dog-ear deformities, the remaining nevus is delicately removed with curved scissors or a scalpel. The wound is closed in two layers using 5.0 Vicryl and 6.0 Prolene. The sutured wound length was measured and compared with the potential wound length of an elliptical excision (Fig. 3). All of the patients were evaluated in outpatient clinics with the Patient and Observer Scar Assessment Scale (POSAS) 3 months postoperatively [7].
RESULTS
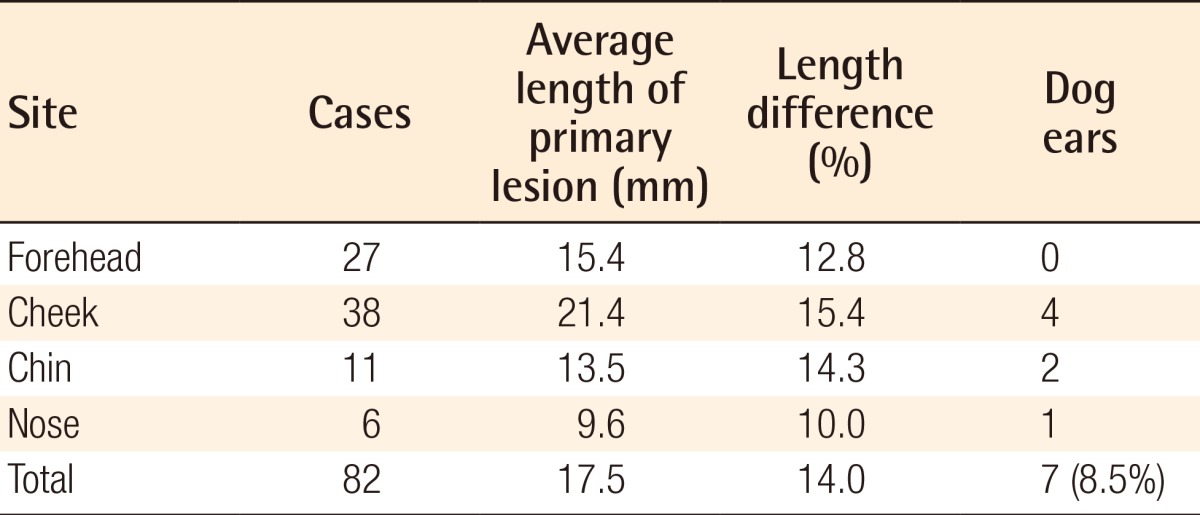
Twenty-seven nevus excisions were conducted on the forehead, 38 on the cheek, 11 on the chin, and 6 on the nose (Figs. 4, 5). The size of the nevi varied between 8 mm and 52 mm (mean, 17.5 mm). Seventy-five of the wounds (91.5%) required no dog-ear repair, 5 wounds (6.1%) required 1 dog-ear repair, and 2 wounds (2.4%) required 2 dog-ear repairs. All of the sutured wounds were shorter than the potential wounds predicted from an elliptical design, and the mean length of sutured wounds was 14% shorter than the expected elliptical wound length (Table 1). There was no significant distortion of normal structures. Complications (dehiscence, hematoma, infection, and skin necrosis) were not observed during postsurgical observation (range, 6-24 months; mean, 10.2 months). All of the scars were deemed aesthetically reasonable based on their POSAS scores.
DISCUSSION
The most common excision skin pattern for nevi is a fusiform or elliptical shape. The usefulness and efficacy of this pattern have been well described in the literature [5,6]. This design allows for the primary closure of the defect without dog-ear deformities. However, there are some significant disadvantages to this technique. One major disadvantage is that the length of the final wound becomes longer than the primary lesion. Commonly, for this design, a length-to-width ratio between 3.0 and 4.5 is recommended. Another disadvantage is the wasting of an excessive amount of healthy tissue to avoid dog-ear deformities. This can create significant aesthetic problems when the lesion is near a critical facial structure, such as an eyebrow, nose, eyelid, or lip. Lastly, the design of this type of incision poorly compensates for the variability in regional tissue laxity.
A dog-ear deformity is a protrusion of soft tissue that forms during wound approximation. It occurs most commonly when a simple elliptical excision is performed with a long axis that is too short compared with the width. The dog ear is more noticeable than the fine linear scar of a well-closed wound. Therefore, elliptical excision without dog ears, even at the expense of lengthening the wound, has traditionally been the most important principle in wound closure [8]. However, this may waste an excessive amount of healthy tissue, and can also result in poor outcomes in both the wound length and direction, as the surgeon plans the design before performing the excision of a lesion. The literature reports considerable variation among planned excisions, wounds, and defect sizes that can be affected by the lesion's location and shape [9]. In addition, several factors influence dog-ear formation including tissue dynamics, wound geometry, surface contour, and surgical technique [10]. Therefore, it is not reasonable to commit to sacrificing healthy tissue prior to measuring the exact shape and size of the defect that will appear after nevus removal. The optimal tissue traction vectors to minimize dog-ear formation can be identified after all possible directions have been assessed. In this manner, we can use adjacent skin with the maximum stretchability.
For wound approximation, usually wide undermining is performed all around the defect. This can help to reduce tension for wound closure, but often brings out some distortion of a nearby critical facial structure such as an eyebrow, eyelid, nose, or lip. In our technique, we perform subcutaneous undermining for tension reduction not in all directions but toward directions opposite of critical structures. This way, we can minimize the distortion of facial structures even though the area for undermining is usually wider than in conventional methods.
Excessive tension in wound closure is a negative factor that can contribute to scar widening or depression. In conventional methods, tension after a nevus excision and primary closure is predicted before operation by examining the elasticity and thickness of the surrounding normal tissue. However, this way, the tension of the sutured wound does not always correspond with that predicted preoperatively. Unfortunately, despite finding out that the tension is excessive, it is not easy to change the plan of a partial excision after the removal of a total lesion. The advantage of our method is that if the tension for approximation is more excessive than what was predicted preoperatively, the width of the excision can be reduced intraoperatively to allow a reasonable level of tension,. Based on our experience, nevi of sizes less than or equal to 3 cm could be successfully excised with this technique. Nevi larger than 3 cm, on the other hand, may require other methods to avoid dog-ear deformity or excessive tension.
The limitations of our study include the lack of validation of our results by a randomized control trial. Although the methods described in our study have been applied successfully to our patients, a larger study with more surgeons may help confirm our conclusions and provide new perspectives.
We believe that, for the excision and closure of facial nevi, this technique should be considered a generally superior method over conventional elliptical excision. Our results also show that compared with elliptical excision, the mean length of the sutured wound was 14% shorter. In addition, this technique has advantages with respect to unnoticeable dog ears, minimal distortion of critical structures, and intraoperative adjustability of the excision width.