With great interest, we have read the publication "The Vacuum Assisted Closure (VAC)-Basket for Easy Fixation of Scrotal Skin Grafts" by Huettinger et al. [1]. The authors describe their experience with a self-constructed vacuum-assisted closure basket for fixation of split-thickness skin grafts in the urogenital area for defect coverage after Fournier's gangrene.
We would like to congratulate the authors for their superior result in the case reported. At our institution, we have long-standing experience in the treatment of defects of the noted area after both traumatic and infectious tissue loss, as we serve as a tertiary referral center providing care for the whole of Western Austria and Northern Italy. In our experience, we feel that following Gillies' principle of reconstructing "like with like" [2] in selected minor scrotal defects such as the one depicted by Huettinger et al. [1], a bilateral thigh lift with permanent fixation sutures to the pubic branches can yield excellent functional and aesthetic results [3]. In case of more extensive defects involving both scrotal and perineal skin loss, we favor split thickness skin grafts for defect coverage. As noted by Huettinger et al. [1], graft fixation remains a challenge. We have developed a VAC fixation technique, the so-called "sandwich technique" [4], that we have used successfully for many years now. We feel that it is well worth sharing with the reader, given its ease of application and superior outcome. We would like to present an illustrative case:
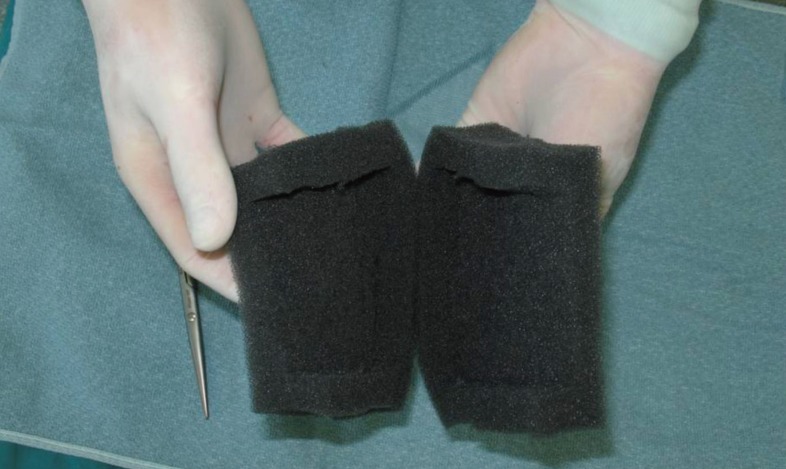
A 47-year-old male was referred to our institution after debridement in the scrotal and perineal area for treatment of Fournie's gangrene in another hospital (Fig. 1). Defect coverage was carried out using bilateral gracilis muscle flaps rotated by 180 degrees around their proximal pedicles. Immediate coverage of the muscle flaps was performed by split-thickness skin grafts (Fig. 2), which were fixed immediately by the aforementioned "sandwich technique" (Figs. 3, 4). The final outcome 3 months postoperatively is shown in Fig. 5.
We agree with Huettinger et al. [1] that VAC fixation in the perineal area provides all-important factors for excellent graft take. With our alternative fixation method, the risk of shearing and tearing forces on the grafts leading to graft loss may be minimized. Our clinical results support this finding.