INTRODUCTION
Brown syndrome is a congenital or acquired ocular motility dis order, characterized by limited elevation in the adduction of the affected eye [1]. It is classified into true sheath and simulated Brown syndrome, based on whether a congenitally short anteri or sheath of the superior oblique tendon is the only cause of the syndrome [2].
Infection, inflammatory disease, and trauma can cause acquired simulated Brown syndrome [3]. It can also be caused by sur gical trauma, glaucoma drainage implantation, ethmoidal sinus surgery, and tucking of the superior oblique tendon [4]. In addi tion, the surgical repair of a blowout fracture can injure the troch lea and superior oblique muscle-tendon complex, which in turn can result in acquired simulated Brown syndrome [5].
We report on three cases of acquired simulated Brown syn drome that occurred after blowout fracture operations and then discuss strategies to prevent and treat such cases.
Case Report
Case 1
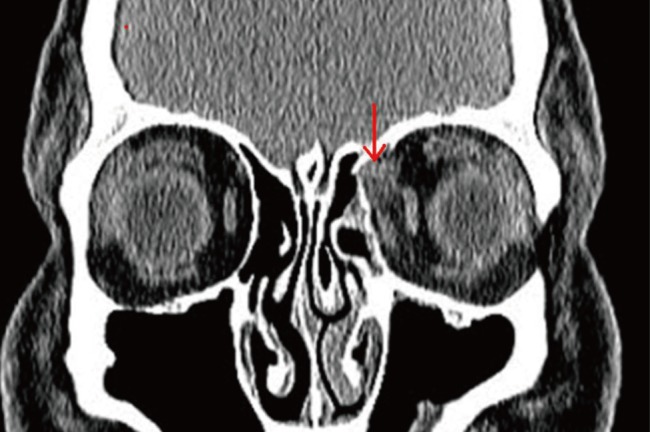
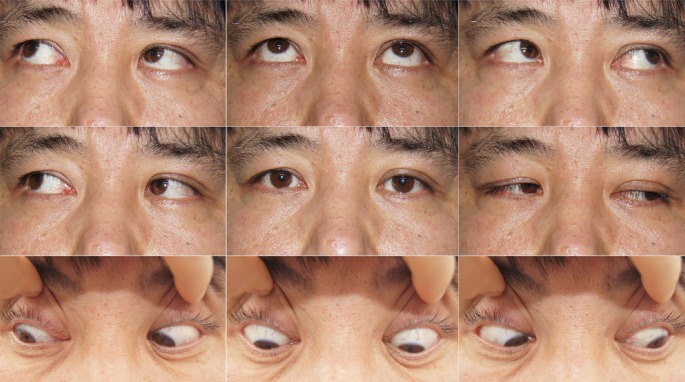
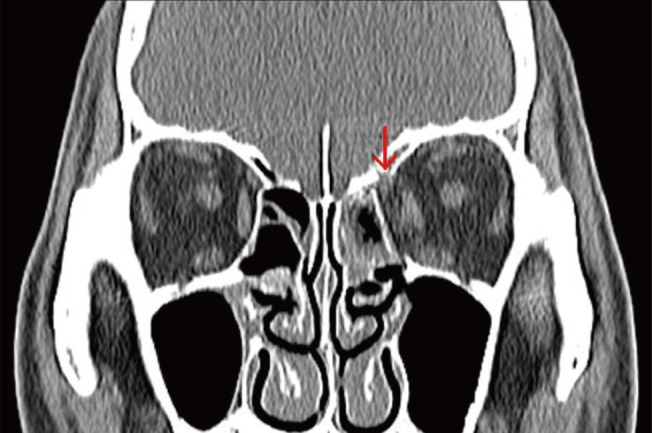
A 37-year-old man visited the emergency room with a left periorbital injury caused by a traffic accident. An initial examination showed no abnormalities in visual acuity, intraocular pressure, or the fundus. The preoperative diagnosis was a blowout fracture involving the medial wall of the left orbit (Fig. 1). Surgical repair of the fracture through insertion of a Medpor (Stryker, Kalamazoo, MI, USA) implant was performed six days after the injury. After the operation, the patient complained of newly developed diplopia. The elevation of the left eye was conspicuously limited during adduction (Fig. 2). A forced duction test of the left eye showed restricted elevation during adduction. A postoperative computed tomography (CT) scan of the orbit showed that the left superior oblique muscle was trapped between the inserted Medpor fragment and the border of the fracture (Fig. 3). Surgical re-exploration was performed and the Medpor implant was removed (Fig. 4). Fortunately, reduction using a bone hook allowed the defect to be almost completely covered with the depressed orbital wall. No artificial bone was inserted. After surgery, a forced duction test showed no restriction of ocular motility. However, the diplopia remained for two months post operatively and was corrected with prism glasses. At an eight-month follow-up visit, the patient's diplopia was alleviated and his ocular motility was significantly improved (Fig. 5).
Case 2
A 52-year-old man came to the hospital with left periorbital blunt trauma caused by a machine tool. He complained of periorbital ecchymosis and subconjunctival hemorrhage without diplopia and ocular motility limitation. An orbital CT scan revealed a left medial blowout fracture (Fig. 6). Surgical repair with the inser tion of a Medpor implant via a transcaruncular approach was performed five days after the injury. Immediately after the oper ation, he complained of diplopia and limited ocular motility. A forced duction test was positive, demonstrating restriction of el evation during adduction of the left eye. A postoperative CT scan showed entrapment of the superior oblique muscle between the Medpor implant and the orbital wall fracture border (Fig. 7). Surgical re-exploration was promptly performed and the entrapped muscle was released by removing the Medpor implant. A new ly designed Medpor implant was reinserted into the depressed orbital wall (Fig. 8). After three month, the diplopia and ocular motility limitation were completely resolved.
Case 3
A 52-year-old man was transferred to our department for the surgical repair of a right medial blowout fracture caused by a violent assault. At first, he complained of diplopia in all directions of gaze. An examination showed limited movement in the right eye during abduction. Traumatic hyphema and vitreous hemor rhage were observed. After the hyphema and vitreous hemor rhage were completely stabilized, an operation was performed to correct the blowout fracture. The herniated orbital fat and muscle were restored and a Medpor implant was inserted into the defect of the orbital wall using a transcaruncular approach. After the operation, he complained of aggravated diplopia and limited ocular motility. Limited elevation during adduction of the left eye was also observed. A postoperative CT scan showed that the superior oblique muscle was compressed by the swell ing of adjacent soft tissue and hematoma. Acquired simulated Brown syndrome was strongly suspected. After two months, the patient's diplopia and limited ocular motility had improved and the patient was satisfied with his condition.
DISCUSSION
In 1950, Brown [6] reported a superior oblique tendon sheath syndrome characterized by limited elevation during adduction. He later redefined this sheath syndrome, dividing it into true sheath syndrome and simulated sheath syndrome [2]. Although the clinical features of true and simulated sheath syndrome are similar, true sheath syndrome is always congenital and persis tent, and does not show spontaneous recovery. In 1975, Parks and Brown [1] reviewed 24 cases of true sheath syndrome, but did not find a tight or heavy anterior sheath surrounding the su perior oblique tendon. The name was then changed to Brown syndrome and the reference to the anterior sheath was dropped [7].
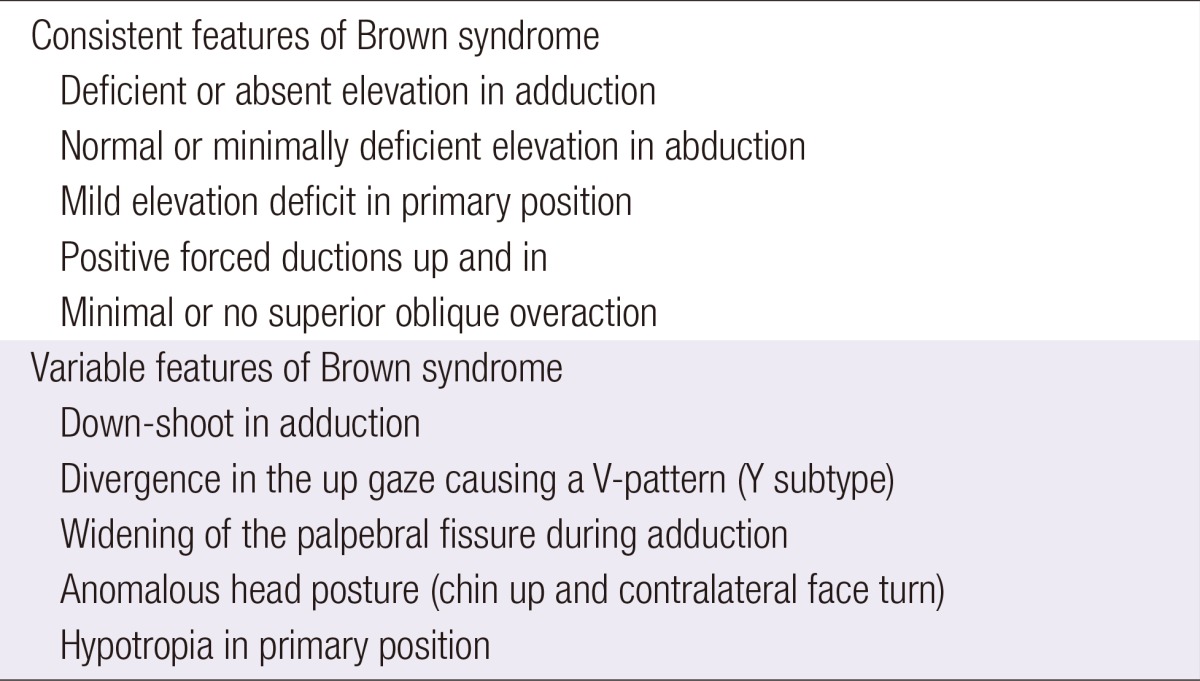
Brown syndrome can be classified as congenital or acquired based on its cause. The cause of congenital Brown syndrome is an anomaly of the trochlear and/or superior oblique tendon, whereas acquired Brown syndrome can be caused by infection, inflammatory disease, trauma, and periocular or sinus surgery [3]. The clinical features of Brown syndrome include limited elevation during adduction, severe limitations in a forced duction examination, lengthening of the palpebral fissure, divergence in the upward gaze manifesting as a V-pattern, and hypotropia in primary position (Table 1) [8]. The differential diagnosis for re stricted elevation during adduction includes pseudo-Brown syn drome, which is caused by paresis of the inferior oblique muscle. Pseudo-Brown syndrome is characterized by a negative forced duction examination, an A-pattern in the upward gaze, ipsilateral superior oblique overreaction, and intorsion in the primary gaze that increases in the upward gaze [9].
Some cases of acquired simulated Brown syndrome after or bital wall fracture operations have been reported. Lauer et al. [10] reported a case of Brown syndrome diagnosed following the repair of an orbital roof fracture. Hwang and Lim [5] de scribed a case of Brown syndrome after the reconstruction of a medial wall fracture and observed that the tendon and muscle fiber near the trochlea were hypertrophied. Seo et al. [4] report ed a case of Brown syndrome after a medial wall fracture recon struction caused by the superior oblique muscle process between an implant and the posterior border of the fracture. Adulkar et al. [11] likewise described a case of Brown syndrome caused by the superior oblique process in a medial wall trapdoor fracture.
Due to the anatomical location of the superior oblique muscle, surgical procedures treating medial blowout fractures are con sidered a potential cause of acquired simulated Brown syndrome. In addition, direct or indirect trauma of the superior oblique muscle, edema, inflammation, and hemorrhage may be involved in the pathogenesis of acquired simulated Brown syndrome [5]. In the three cases reported here, the patients had impaired ocu lar motility involving limited elevation during adduction as well as positive forced duction examinations. When orbital CT scans were performed, we observed that the superior oblique muscle was trapped between the Medpor implant and the fracture mar gin. This condition is sometimes difficult to differentiate from inferior oblique paresis, but can be confirmed with a positive forced duction test. Once muscle entrapment is confirmed, prompt surgical release is essential because the muscle may later be fibrosed by cicatricial adhesions.
The surgical reconstruction of a blowout fracture involves a risk of external ocular muscle entrapment [12]. Therefore, it is essential to determine whether the external ocular muscle is trapped between the inserted implant and the fracture margin. Superior oblique muscle entrapment is uncommon and is there fore seldom considered a possibility during the identification of the superior margin of the medial orbital wall. The surgeon should always consider the possibility of Brown syndrome if an implant is put in place without clearly identifying the fracture margin, and also should perform a forced duction test after inserting the implant in order to ensure that all extraocular muscles were re leased.