INTRODUCTION
Recently, minimally invasive approaches such as transoral robotic surgery have been developed for the management of oropharyngeal cancers [
1]. The parapharyngeal space (PPS) is a difficult area to access due to its anatomical complexity and relationship with the surrounding vital structures, such as the carotid artery, internal jugular vein, and cranial nerves IX to XII [
1]. Pollei et al. [
2] suggested that the exposed branches of the external carotid artery must be ligated in the resection bed and coverage should be achieved with local flaps or surrounding tissues, typically including the lingual and facial arteries in oropharyngeal resections.
Reconstruction of oropharyngeal defects after resection of oropharyngeal cancer is a significant challenge for the reconstructing surgeon in terms of ensuring favorable functional and esthetic outcomes. Oral cavity defects after tumor resection can be reconstructed depending on the size and anatomic position of the defects. Traditionally, the oral cavity defects resulting from tumor resection were reconstructed using skin grafts, locoregional flaps, and free flaps [
3]. Ideal reconstruction should be accomplished by matching the resected tissue in texture, color, consistency, bulk, and minimal donor site morbidity. In addition, the flap should be easily harvested and versatile [
4].
Many surgeons have described the use of intraoral local flaps from the oral mucosa. Currently, they use a buccinator myomucosal flap [
5] based on the buccal artery, and a facial artery and a buccal fat pad flap [
6] for the reconstruction of oropharyngeal defects. However, to date, there have been no published data on the reconstruction for lateral oropharyngeal defects by using two flaps, namely a buccinator myomucosal flap and a buccal fat pad flap. Therefore, the purpose of this study was to introduce our reconstructive technique and novel use of a combination of the buccinator myomucosal flap with a buccal fat pad flap to cover defects of the lateral oropharyngeal wall after cancer excision and to discuss the associated anatomy, surgical procedure, and clinical applications. In addition, we present the anatomic and cadaveric foundations for the buccinator myomucosal flap and the buccal fat pad flap for reconstruction of the lateral oropharyngeal wall.
RESULTS
All flaps were harvested and transposed successfully. The largest oropharyngeal defect measured 6 cm×4 cm (length×width). The largest buccinator myomucosal flap measured 5 cm×2 cm (length×width), and the length of the flap pedicle was 4.5 cm. The largest buccal fat pad flap measured 6 cm×2 cm (length× width). The flap was rotated about 180° inferiorly or superiorly and then fixed without any tension. The width of the donor site was as large as 2 cm, so the site was closed primarily.
The flaps were completely epithelialized after four weeks. The patients were followed for at least six months. There were no flap failures or postoperative wound complications. All patients tolerated a normal diet, and no patient had problems related to mouth opening, swallowing, or speech.
Case 1
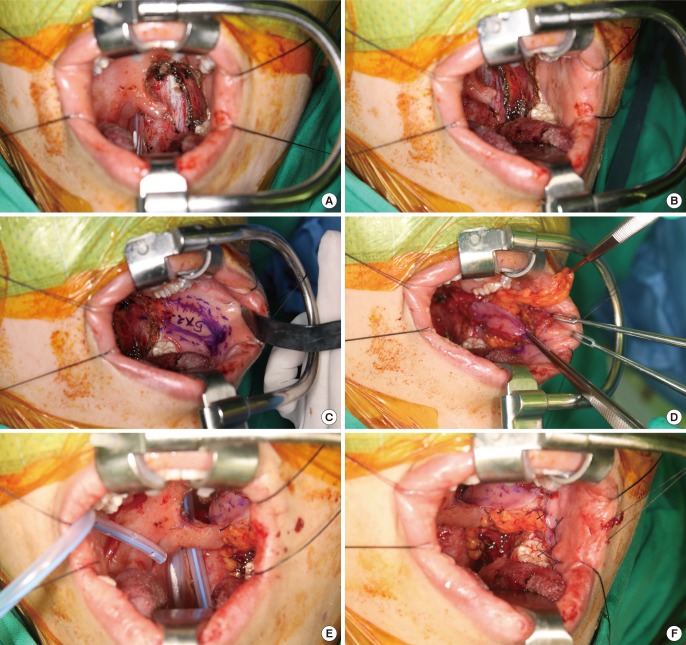
The patient was a 32-year-old woman with squamous cell carcinoma (T2N2M0) of the left tonsil. The patient underwent lateral oropharyngectomy and modified radical neck dissection to preserve the facial artery. The oropharyngeal defect measured about 4 cm×1.5 cm, and the carotid artery was exposed. The oropharyngeal defect was reconstructed using a combination of a buccinator flap and a buccal fat pad flap. The size of the buccinator myomucosal flap measured about 5 cm×2 cm as did the buccal fat pad flap. The flap was transposed inferiorly and covered the defect. The donor site was primarily closed (
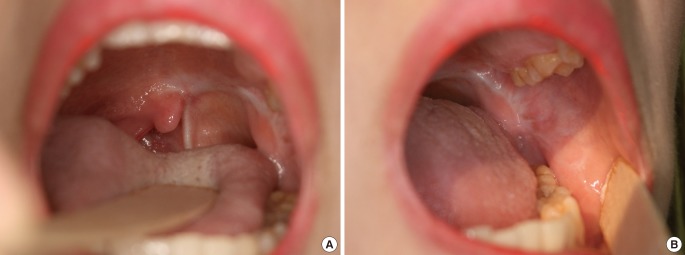
Fig. 1). The flap was completely re-epithelialized after four weeks. No infection or flap resorption was observed after ten months of follow-up (
Fig. 2). She had no limitations with respect to mouth opening or trismus. The aesthetic results were good without cheek depression.
Case 2
The patient was an 81-year-old man with squamous cell carcinoma (T2N2M0) of the left tonsillar fossa. The patient underwent lateral oropharyngectomy and modified radical neck dissection to preserve the facial artery, accessory nerve, and internal jugular vein. The oropharyngeal defect measured about 4 cm×2 cm, and the tortuous internal carotid artery was exposed. The oropharyngeal defect was reconstructed using a combination of the buccinator myomucosal flap and the buccal fat pad flap. The buccinator myomucosal and buccal fat pad flaps were each about 5 cm×2 cm. The flap was transposed inferiorly and covered the defect. Some of the donor site was closed, and the remaining area was left open with the expectation of secondary healing.
The flap and the donor site were completely re-epithelialized after four weeks. No wound complications such as infection or resorption of the buccal fat pad were observed after nine months of follow-up. He had no limitations in oral function (e.g., mouth opening or trismus). The aesthetic results were good without visible scars.
Case 3
The patient was a 65-year-old man with squamous cell carcinoma (T4N2M0) of the right palatine tonsil. As the tumor was adjacent to the internal carotid artery, he underwent neo-adjuvant chemotherapy for 16 weeks. He subsequently underwent lateral oropharyngectomy and modified radical neck dissection to preserve the facial artery. The oropharyngeal defect measured about 6 cm×4 cm, and the internal carotid artery was exposed. The oropharyngeal defect was reconstructed using a combination of the buccinator myomucosal flap with the buccal fat pad flap. The buccinator myomucosal flap measured about 5 cm×2 cm, and the buccal fat pad flap measured about 6 cm×2 cm. The flap was transposed inferiorly and covered the defect. Some of the donor site was closed, and the remaining area was left open with the expectation of secondary healing.
A minor wound complication occurred, and a revision was done. The flap and the donor site were completely re-epithelialized after four weeks. There were no wound complications including infection or resorption of the buccal fat pad after six months of follow-up. The patient was able to open his mouth without difficulty and had no trismus.
Cadaveric study
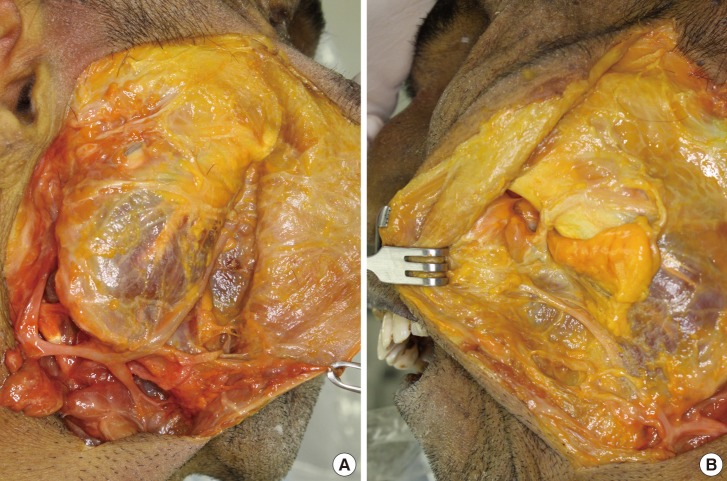
The anatomy of the buccinators, buccal fat pad, and facial vessels has been extensively described. In brief, the facial artery branches from the external carotid artery and enters the face by crossing the inferior border of the mandible and ascending toward the nasal alae. The facial artery supplies the buccinator muscle through inferior and anterior buccal branches and ascends in the nasofacial groove to the medial canthus as the angular artery (
Fig. 3A). The anastomoses among arteries supplying the buccinators muscle could not be found in our cadaver, as was in our cadaver. The facial artery and vein were in close proximity to the angle of the mandible. The buccal fat pad flap were encapsulated and distinct from the subcutaneous fat. Its dissection was performed by mobilization of its body and buccal process on a vascularized pedicle (
Fig. 3B).
Through the intraoral incision (
Fig. 4A), the buccinator myomucosal flap was elevated in the cadaver without injury to the orifice of the parotid duct. The pedicle of the facial artery was not skeletonized or included in the flap because of the preservation of the blood supply network (
Fig. 4B). The buccal fat pad flap was then elevated in the same operative field (
Fig. 4C). The flap was long enough to translocate the buccal fat pad flap to the lateral oropharyngeal defect (
Fig. 4D, E).
DISCUSSION
Several methods for oropharyngeal reconstruction secondary to cancer resection have been described. The choice of treatment depends on many factors such as the size of the defect, the position of the defect, the volume or condition of surrounding tissue, functional restoration, and aesthetic results. No reconstruction is needed for small defects because they heal spontaneously or can be closed primarily.
Several prior studies described skin grafts and locoregional flaps for reconstruction of moderately sized defects of the oral cavity [
89101112]. Although a split thickness skin graft is simple to harvest, is thin, and can be applied to a large defect, it can result in contractures that interfere with the restoration of normal oral functions such as mouth opening and cannot be used to cover exposed vital structures such as bone and vessels [
13]. Vital structures such as carotid artery, jugular vein, and cranial nerve are often exposed after oropharyngectomy. In a situation where the exposed structure is not completely covered, postoperative bleeding can occur. Pollei et al. [
2] reported that postoperative bleeding occurred in 5.4% of the patients with 67.3% of them requiring operative intervention, and severe life threatening bleeding occurred in 1.1% of the patients. Therefore, adequate coverage of critical structures is a key component of defect reconstruction.
The disadvantages of locoregional flaps include the limitation in size of the flap supplied with a certain pedicle and postoperative contractures, which can result in limited mouth opening, trismus, and donor site morbidity. Reconstruction using a locoregional flap is not appropriate for moderate-to-large defects. Defects, too large for primary repair, can be reconstructed using free flaps. Free flaps are the first choice for complex intraoral reconstructions involving the tongue, floor of the mouth, palate, cheek mucosa, and lip [
1415]. Although free flaps are the best choice for large defects, there are several disadvantages in terms of flap bulkiness, donor site morbidity, and long and complex surgery. The ideal reconstruction should completely cover the defects and replace the original tissue with the same or similar type of tissue. The reconstructed tissue should be similar to the native tissue in terms of mucosal sensitivity, volume, and texture [
16].
The buccinator myomucosal flap and the buccal fat pad flap are suitable options for covering a buccal defect. The buccinator muscle is a thin, rectangular-shaped cheek muscle that is involved in actions such as whistling, sucking, and mastication [
4]. At its medial aspect, the buccinator muscle is covered with the mucosa and submucosa of the cheek, and at its lateral aspect, it contacts the mandible, masseter muscles, buccal fat pad, and buccopharyngeal fascia [
3]. The buccinator muscle has a rich blood supply from the network between the facial and the buccal arteries [
17]. Zhao et al. [
18] reported that a buccinator myomucosal flap can be harvested as a pedicled flap or axial flap based on the buccal or facial artery and can be based anteriorly, posteriorly, or superiorly. The posteriorly based flap is useful for the coverage of the tonsil bed, soft and hard palate, and retromolar trigone, while the anteriorly based flap is good for the reconstruction of the lip, floor of the mouth, and tongue. The superiorly based flap has been described in the repair of defects in the anterior hard palate, alveolus, and lips, as well as the orbit. However, this flap is limited by the size and volume needed to cover the defect.
The buccinator myomucosal flap has several advantages. It has great versatility for reconstructing small-to-moderately sized intraoral defects, can be flexibly designed in various shapes, and has minimal donor site morbidity with minimal scarring due to the possibility of closure with sutures. Most importantly, it is similar to the original tissues in terms of texture, color, and sensitivity. The buccinator flaps maintain mucous secretion and sensitivity and oral functions such as speaking and swallowing [
16]. Harvesting the flap is technically easy as compared to free flap harvest, so the operating time is shorter than that of reconstruction using free flaps or local flaps.
Egyedi [
19] suggested the use of a buccal fat pad flap for intraoral reconstruction. The buccal fat pad is an encapsulated, complex, three-dimensional structure with neurovascular bundles, distinct from the subcutaneous fat [
20]. It lies between the buccinator muscle and the masseter muscle [
3]. The flap can be applied to reconstruct defects of the hard palate, soft palate, buccal mucosa, and posterior maxilla [
21]. It has a rich blood system sufficient for the coverage of a small-to-moderately sized oral defect. In addition, the buccal fat pad flap is flexible to design, is simple to access, has low morbidity, and has excellent re-epithelization [
22].
Few studies have described the combination of a buccinator myomucosal flap with a buccal fat pad flap [
22]. In our experience, the use of a buccinator flap alone was limited in terms of the length and volume of the flap for defect coverage. Furthermore, while the buccal fat pad flap was sufficient with respect to size or volume, the fat tissue was vulnerable to tension or external forces. Thus, we used the buccinator flap with the buccal fat pad flap for the coverage of oropharyngeal defects in this study.
In our cases, after tumor removal, the largest oropharyngeal defect noted measured 6 cm×4 cm with the internal carotid artery exposed. As previously stated, the mean pedicle length of buccinator myomucosal flaps ranges from 4.2 to 5.5 cm, and the paddle size of the flap ranges from 2.2 cm×2.1 cm to 3.5 cm×3 cm [
7]. In order to obtain a sufficient flap volume and length, we used the combination of a buccinator myomucosal flap with a buccal fat pad flap. This approach provides additional available tissue volume for defect coverage, allowing larger defects to be reconstructed than with the use of any flap alone.
In the process of flap design, the width of the flap was not to exceed 2.5 cm for primary closure. The opening of Stenson's duct was preoperatively marked with a suture to avoid damaging it.
Incision and dissection are both needed when using a buccinator flap or a buccal fat pad flap. When using a buccinator myomucosal flap and a buccal fat pad flap together, the operative field is the same. After elevation of the buccinator flap, only simple dissection is needed to elevate the buccal fat pad flap from the exposed raw surface. The use of these flaps for the same reconstruction has several advantages including an easy, relatively fast surgery and intraoral harvest.
During elevation of the flap, we were focused on the dissection of the pedicle to preserve blood supply to the entire flap. The artery and vein surrounding the buccinator muscle organized the complicated blood network. The buccinator muscle has a rich blood system from the anastomosis between the facial artery and the external carotid artery, the posterior buccal branch of the facial artery, the internal maxillary artery, the buccal artery, and the posterosuperior alveolar artery. In addition, the vein drains into the buccal venous plexus, the pterygoid plexus, the internal maxillary vein, and the deep facial vein [
18]. During elevation of the buccinator flap, the pedicle was not clearly identified and the vascular pedicle should be just wide enough to be rotated on a pivot point in order to maintain the blood supply network because the blood supply and the venous drainage of the flap come from the network of small arterioles and venules.
The blood supply to the buccal fat pad flap is mostly through a network of vessels surrounding the capsule. Therefore, the surgeon must take care to keep the capsule and vessels intact during dissection of the flap. Subsequently, a part of the capsule is separated to obtain sufficient length in a range that does not interfere with the blood supply. The flap was rotated about 180° to cover the defect. The direction of the rotation was either superiorly rotated or inferiorly to avoid kinking of the pedicle and tension.
Because of the tiny diameters of vessels in the cadaveric study, there were no networks of blood vessels found around the buccinator flap and the buccal fat pad flap. However, it is certain that not skeletonizing the pedicle of the flap and preserving the network of vessels are helpful for the transposition of the buccinator flap and the buccal fat pad flap. In two different specimens, we found that the lengths and volumes of the buccinator flap and the buccal fat pad flap are sufficient to cover the lateral oropharyngeal defect.
Dissecting the buccal area always involves the risk of facial nerve trunk damage. However, when we checked the location and depth of the flap in the cadaver, damages to the digital buccal branches seemed possible, while direct damages to the trunk itself seemed very unlikely.
Our study has several limitations. The main limitation is the small number of the patients who underwent oropharyngeal reconstruction using the buccinator flap with the buccal fat pad flap. While other studies utilized a skeletonized pedicle in defect reconstruction, in our study, we determined that the pedicle was wide enough to maintain appropriate blood supply, and no complications occurred. Further studies with an anatomic and cadaveric foundation should be done to characterize the blood supply system. A compilation of more cases and cadaver specimens will aid a deeper understanding of the buccinator and buccal fat pad flaps.