Hydatid disease is a parasitic infestation that is caused by the cestode Echinococcus granulosus (E. granulosus) that has a higher prevalence in South American, Mediterranean, Middle Eastern, and East Asian countries. Humans are incidental intermediate hosts because of the ingestion of embryonated eggs in food contaminated with dog feces. In humans, the liver and the lungs are the most commonly affected sites of the body; the other sites include the peritoneum, spleen, kidney, uterus, and pancreas [1]. A solitary subcutaneous hydatid cyst is extremely rare. In a different series, the frequency of subcutaneous tissue involvement was approximately 2%; however, primary lesions without secondary damage to any organs have been very rarely reported [2]. We herein present an unexpected and uncommon etiology of a subcutaneous cyst diagnosed as a hydatid cyst, which might be of interest to surgeons.
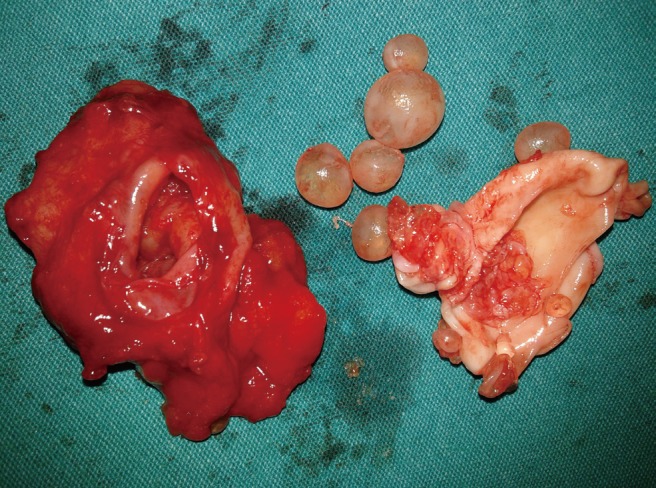
A 66-year-old man was admitted to our department with a subcutaneous mass on the right side of the thoracic region. He had no complaints but the mass with palpation. On the ultrasonography (USG), a complex, cystic lesion (44×21 mm) with septate in the subcutaneous adipose tissue was detected. Upon the clinical diagnosis of the subcutaneous cyst, the patient underwent surgery under local anesthesia. Multiple small cysts in a larger cyst wall were observed intraoperatively; this suggested the presence of a hydatid cyst (Fig. 1). Total cystectomy was performed (Fig. 2), and the cyst was cleaned with hypertonic saline. Histopathological examination confirmed the diagnosis of the hydatid cyst. Serological tests were negative for the Echinococcal antigens. No abdominal pathology was seen on the USG. The patient was started on an oral albendazole treatment for 3 months. On follow-up, no recurrence was observed.
Hydatid disease is a zoonosis caused by the larval stages of E. granulosus; this disease is often underdiagnosed because of its silence; it usually develops over the years and does not become symptomatic until a compression of the internal organs occurs. A hydatid cyst can be found anywhere in the human body, particularly in the liver and the lung and rarely on the other sites. A subcutaneous location is extremely rare when the cyst is primarily diagnosed without any involvement of the liver or any of the abdominal organs, which causes its route to remain unknown.
Goyal et al. [3], in their retrospective study from India, an endemic country, reported the fine-needle aspiration records of their 5,954 patients who had superficial palpable nodules. They found that 41 cases (0.68%) were diagnosed as parasitic lesions on cytology, and among these, one case of hydatid cyst was observed [3]. In their study, all cases had lesions measuring from 0.5 cm to 4.5 cm except the hydatid cyst, which was 11 cm in size [3]. This may be due to the asymptomatic and slow growth characteristics of the hydatid disease unless the cysts have a pressure effect on the surrounding tissue. It was reported that the annual growth rate of the cyst is about 1-3 cm in diameter [1].
Ultrasonography is useful in the diagnosis, showing the size, localization, and type of cyst with a sensitivity of 95%, and if vesicular fibrils are present, the sensitivity increases up to 100% [4]. Serological tests can also be useful in the diagnosis; however, most of the subcutaneous hydatid cysts give negative results [4].
The best treatment option is complete surgical excision without any leakage of the cyst content to the surrounding tissue as such a leakage can cause anaphylaxis and local recurrence; however, in our case, the cyst rupture occurred without any anaphylaxis, which may mostly occur at the time of peritoneal contiguity. Further, the cyst pouch should be irrigated with antiscolicidal solutions.
In conclusion, parasitic etiology should be considered an important differential diagnosis of soft-tissue nodules, particularly in endemic regions, and the surgeon should be aware of hydatid cysts in the case of a diffuse, cystic, slow-growing mass.