Systemic lupus erythematosus (SLE) is a relatively common entity in rheumatology. Skin involvements such as nodules, vasculitis, and calcifications are commonly reported in patients with SLE [12]. In our center, we encounter many rheumatoid patients referred from our rheumatology clinic. However, the case shown here was very unusual even to our experienced eyes.
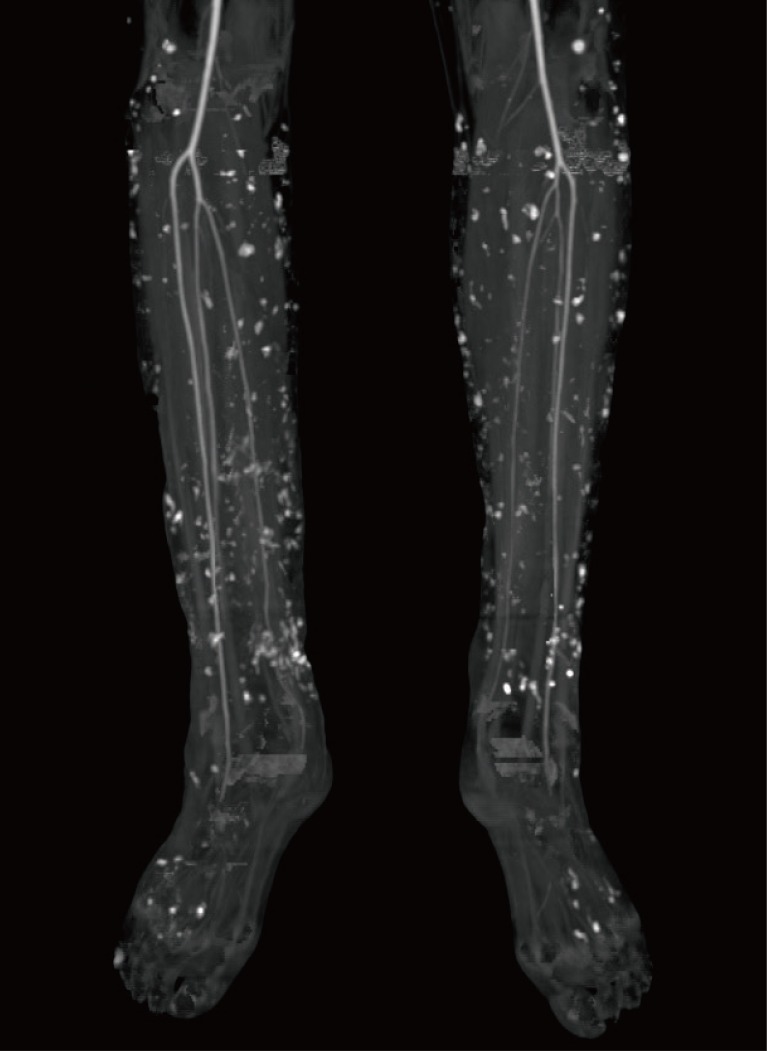
A 37-year-old female patient, who had suffered from SLE for 16 years, had acquired progressive calcifications on the entirety of both of her legs. The calcification lesions were initially not severe and were limited to the lower leg area. However, the progression accelerated into groups of calcifications on both legs, which resulted in multiple leg defects (Figs. 1, 2). Her computed tomography (CT) angiography clearly showed the extent of the disease (Fig. 3). To help heal the wounds, immune suppressive drugs were administered, but the patient's condition was serious. Though administration of intravenous immunoglobulin was temporary effective to control the SLE, the wounds worsened, which led to sepsis. The wounds progressed despite our efforts. We serially debrided the infected defects and covered the defects with free flaps and 0.010-inch split-thickness skin grafts from the thighs (Fig. 4). Up to the present, a total of 18 surgical procedures have been performed. The wounds are now stable with conservative treatment.
Calcifications with this extent of progression in a SLE patient are extremely rare [3]. Nevertheless, this case reminds us that we should not overlook skin involvements associated with SLE, especially progressive calcifications, which can lead to serious morbidities.