INTRODUCTION
Female hairline correction surgery is gaining popularity among East Asians, who characteristically have brachycephalic facial features [1] for which face slimming cosmetic surgery has been developed. Unlike Caucasians, most of whom request frontal hairline lowering surgery, East Asians usually request adjustment of their side-hairline from the frontotemporal recess area all the way down to the sideburn. Such hairline correction is mostly requested by individuals with the characteristic brachycephalic facial characteristics.
The thick, black hair that is characteristics of East Asians, inevitably results in thick hair being transplanted to the hairline area, which can lead to an unnatural look that makes it obvious that surgery has been performed. Even when a 10× magnification microscope or magnifying loupe is used to measure a participant's hair and select the thinnest hair follicular units to transplant to the frontal area, such an unnatural look is difficult to avoid if the participant's hair is comparatively thick all over.
To our knowledge, there are few reports on techniques for solving this problem by thinning the transplanted hair. Thus, we here report good results of hair thinning by intense pulsed light (IPL) together with a review of relevant published reports.
METHODS
This study was approved by the Internal Institutional Review board of the Korea National Institute of Bioethics Policy (IRB No. 2015-0287-001).
IPL was used to thin the hair of 54 black-haired Korean women who had undergone hairline correction surgery and who, despite being satisfied with the overall shape and density of their hairlines, believed they looked unnatural because their naturally thick hair had been transplanted to their frontal hairlines.
The mean age of the study participants was 31.2 years (from age 22 to 46) and the mean interval since hairline correction surgery 2.1 years (from postoperative 10 months to 5 years at most). Participants with female pattern hair loss or who had undergone surgery that could have affected the hairs along the frontal hairline were excluded from the study. Patients with the following conditions were excluded from the study: pregnancy, menopause, and any other health conditions that could have a harmful influence on the hair follicle such as severe weight loss.
Medical records and photographs were reviewed retrospectively. Hair shaft diameter was measured with a micrometer (Mitutoyo, Kawasaki, Japan) during pre-procedure, and at 4-month and 1-year post-procedure.
The area of surgery was determined by detailed discussion with the participants and the target of thinning, characteristically the three to four most frontal lines of hair, identified.
Hair thinning was achieved by using an Intense Pulsed Light system (R2PL, Ahwon, Bucheon, Korea).
Treatment protocol
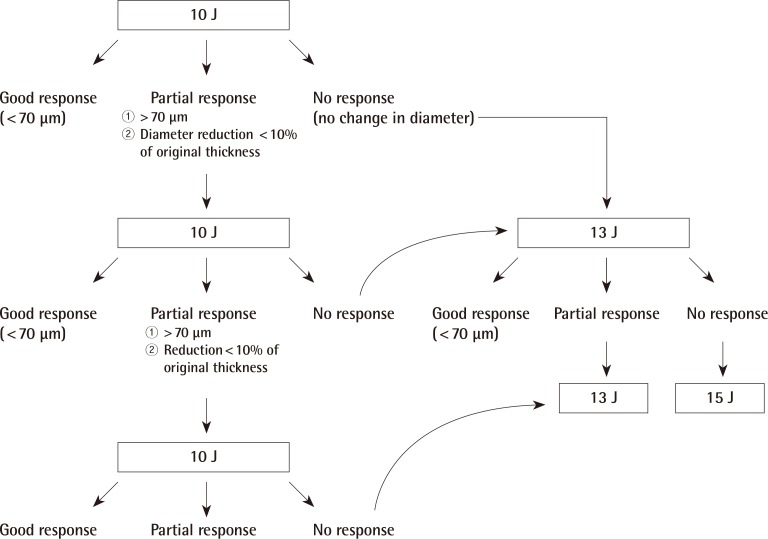
In the initial treatment, 10 J was administered. The parameters were as follows: energy, 10 J/cm2; duration, 30 ms; wavelength, 695 nm filter. Follow-up 4 months post-procedure, responses to treatment were categorized as good, partial, or no response on the basis of hair thickness change and subject's subjective opinion. A decision was then made on whether to perform one or more additional sessions. Those with no detectable changes in hair thickness after the first session were categorized as having no response and were administered 13 J in a second treatment session. Those who requested additional thinning and were categorized as having partial responses; namely, those with some change in hair diameter but with hair diameter still exceeding 70 µm or a decrease of ≤10% in hair diameter, were administered 10 J in a second treatment session (Table 1).
Responses were reassessed 4 months after the second procedure. Participants who were classified as having partial responses were to be administered 10 J in a third treatment session. Those with no response after the second session were to receive 15 J in their third treatment sessions.
Ten thick anagen hairs were randomly selected from the area of photo epilation by an expert hair surgeon using 5x loupes.
Hair shaft diameter was assessed pre-procedure, and 4-months and 1-year post-procedure; additionally, 12 participants were followed up for more than 3 years.
Satisfaction was scored on a scale of 1 to 5 (1, very dissatisfied; 2, slightly dissatisfied; 3, neutral; 4, relatively satisfied; 5, very satisfied) by 54 patients on 1 year follow up.
RESULTS
Pre-procedure mean hair thickness of total 54 patients was 78.86 µm. The procedure was conducted on an average of 1.6 times, and the mean reduction in hair diameter was 16.2%. Forty of 54 subjects (74%) achieved satisfactory hair thinning with only one procedure. The measured thickness was 66.43 µm at the end of the first year in patients who were satisfied after one procedure. Thirteen cases achieved satisfactory hair thinning after two sessions. Mean thickness was 74.44 µm and 67.51 µm, before and after the second session. One case required a third session with 15 J, thinning from 89.00 to 66.50 µm.
Good response group after first session
Good response group (40 patients) achieved hair thinning from 78.01 to 66.14 µm after treatment.
Partial response group after first session
For partial response group (3 patients), hair thickness was 82.03 µm prior to treatment and 72.33 µm after treatment. After second procedure with 10 J, the average hair thickness was 63.33 µm.
No response group after first session
Hair thickness for no response group (11 patients) was 80.36 µm before procedure and 81.09 µm after procedure. Ten out of the eleven patients showed good response with 13 J on second session. Hair thickness after the first session was 79.70 µm and after second procedure was 66.00 µm on average.
A third treatment was administered to the single participant who did not achieve satisfactory thinning after the second session. This 36-year-old woman had undergone hairline correction surgery in another hospital 3 years previously and presented to our clinic requesting hair thinning treatment. She had a very thick initial hair diameter (89.00 µm). Her mean hair thickness was 82.00 µm after the second session and 66.50 µm after the third session, in which she received 15 J. She was satisfied with this result.
The mean patient satisfaction score was 4.3. The satisfaction score was 4 or higher in all patients (range, 4–5).
There were no serious complications such as hypopigmentation, infection or post-treatment scarring. Temporary mild erythema and swelling occurred within 2–3 days post-procedure but these symptoms quickly resolved. One participant reported mild pain in the procedure area up to the following day but this resolved with nonsteroidal anti-inflammatory drugs.
There were no significant changes in hair diameter at 4 months and 1 year after the procedure. The mean duration of follow-up was 14 months (range, 11–54 months). In the twelve participants who were followed up for more than 3 years, hair thinning was maintained.
Representative case
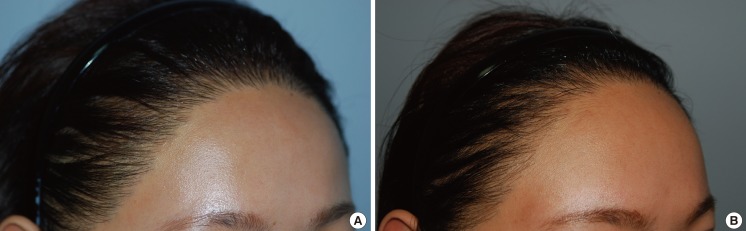
A 31-year-old woman who had undergone hairline correction surgery 19 months previously visited our clinic because of the thick and unnatural appearance of her frontal hairline. Her pre-procedure hair thickness was 75.65 µm and she received only one session of IPL. Her hair thickness was 64.05 µm and 65.40 µm at 4 months and 4 years post-treatment, respectively (Fig. 1).
DISCUSSION
Hairline correction surgery in East-Asian individuals mostly focuses on making the face appear more slimmer by making changes in the area from the fronto-temporal recess to the temple, infra-temple, and sideburn areas [1]. Despite minimal mismatching of thickness, direction and angle of the transplanted hair, such side-hairline surgery can easily lead to an unnatural look that makes it obvious that surgery has been performed. This is partially attributable to the unique characteristics of East Asian participants' hair [2]: East Asians have the lightest skin color of all Asians and their hair is characteristically thick and coarse. Their hair density is also very low compared with that of Caucasian individuals. Thus, achieving satisfactory results with hairline correction surgery is very difficult in East Asian women. Even when thin hair follicular units have been placed in the frontal hairline area, if the pre-procedure overall hair thickness is >75–76 µm, thick hairline hair is very noticeable and it is obvious that the individual has undergone cosmetic surgery.
Both the thickness of preexisting hairs in the frontal hairline and occipital area are important: hair transplanted into the newly shaped hairline appears thicker than otherwise if there is a considerable difference in thickness between the frontal and occipital hair. Minimizing the width of the transplanted strip and maximizing the length of the strip to reach the temple area, or obtaining the donor hair from the lower occipital area, can help in making the transplanted hair appear thinner. However, these strategies are relatively ineffective if the hair is comparatively thick overall. In all such cases, our procedure for hair thinning can be very useful.
Laser epilation for hair thinning can be done a year after hairline correction surgery because it takes about a year for the new implanted hair to grow to a sufficient length.
IPL has been used for medical purposes for many years [34]. “PhotoDerm” (ESC Medical Systems, Needham, MA, USA), the first commercially available IPL system, was approved for treating vascular lesions by the U.S. Food and Drug Administration in 1955 [5]. Various IPL products were subsequently released, and most are currently being used to treat pigmentation disorders and epilation [6]. The main targets of IPL treatment are chromophores such as melanin in the skin and oxyhemoglobin, which is predominantly found in clinically red lesions. Epilation can be treated with a 600–950 nm wavelength, melanin being the target chromophore. The light administered by low fluence photo-epilation with IPL is changed into heat energy that selectively destroys the melanin-containing part of hair bulb, transforming it into a catagen-like phase [3].
Hair that regrows after ruby and diode laser treatment is reportedly thinner and lighter in color than prior to the treatment. Lin et al. [7] and Grossman et al. [8] have reported that these changes result from selective destruction of thicker and/or darker hair, laser-induced changes in the hair growth cycle that affect hair diameter, and incomplete destruction of stem cells, follicular matrix and/or dermal papillae. Roosen et al. [9] have also described temporary photo-epilation after IPL treatment reporting that partial or complete regrowth occurs about 12 weeks after such treatment, which does not result in any destruction of the stem cell region.
Park et al. [10] have reported the results of using long-pulse neodymium-doped yttrium aluminum garnet therapy to achieve fine hair after hairline correction surgery in women. However, they did not provide long-term follow-up data, their mean duration of follow-up being only 6.3 months. In addition, their target hair diameter was 50–60 µm. The authors believe that 65 µm is a more appropriate target, this being sufficiently thinner than the characteristic 70–80 µm of the occipital donor hairs that are used for transplantation of the frontal hairline area. In practice, few participants request additional hair thinning when their foremost frontal hairs are 60–68 µm thick. Thus, women whose donor hair diameter is within this range do not require hair thinning after hairline correction surgery.
In our opinion, a 65 µm target is optimal for East Asian women who have undergone hairline correction surgery, 70–74 µm being considered moderately thick, 74–78 µm rather thick, and in excess of 78 µm very thick. If the hair is thinned to <60 µm, it can appear too thin, resembling vellus hair. The resultant pronounced difference in thickness between the hairs immediately posterior to the procedure area and the more anterior newly implanted hairs can thus result in an unnatural look.
We used a lower output than that required for epilation, our aim being to achieve sufficient damage to reduce the thickness of the hair follicle without destroying it. There was no difference in hair thickness between 4-month and 1-year post-procedure in participants with successful thinning. We thus concluded that thinner hair grows in 2 to 3 months after partial IPL-induced damage and that most of the newly grown hairs have reached their final thickness within 6 months after IPL.
The key factor in hair thinning by IPL is to avoid complete hair ablation. The Ahwon IPL system used in this study is set at 25 J for hair removal. We used 10 J, which is 40% of that setting, in the initial session. To avoid inducing complete ablation of transplanted hair, the power used in subsequent treatments should be gradually increased from 10 J. When considering administering subsequent treatment, we recommend following the algorithm shown in Fig. 2, which requires categorizing the response to treatment as: good, partial, and no response (Fig. 2).
A limitation of the current study was the relatively short follow-up period. Even if we report on three or more years of follow-up in 12 patients whose hair thickness remained consistant with the one-year follow-up results, a long-term follow-up study with a larger sample size is necessary.