When flap failure occurs in bilateral breast reconstruction, surgeons need to deal with the situation effectively in order to optimize the prosthetic reconstruction and to make the bilateral reconstruction successful [1].
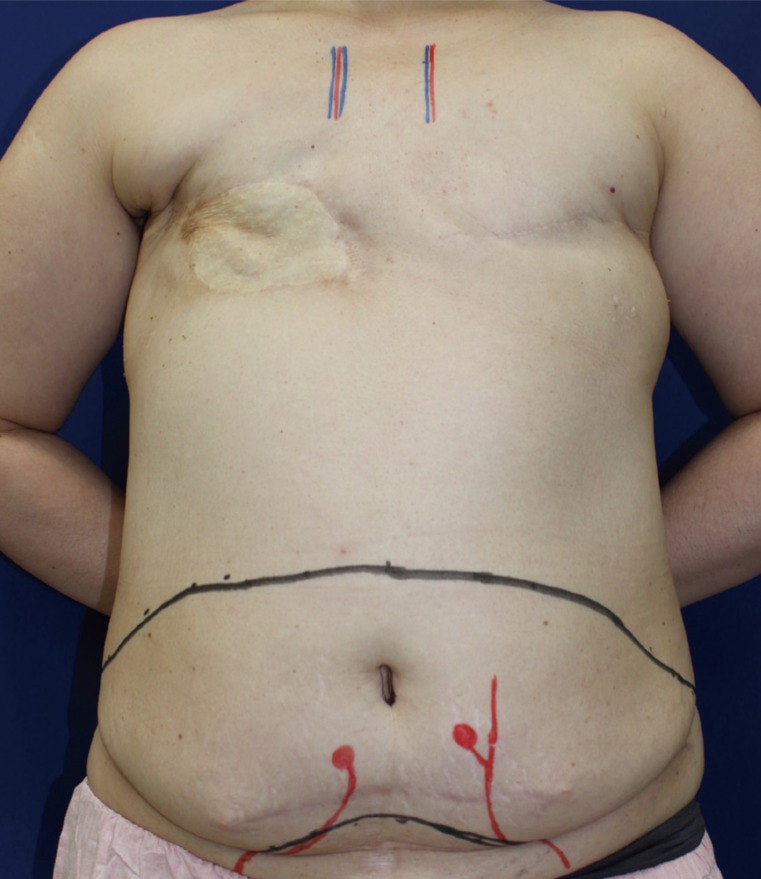
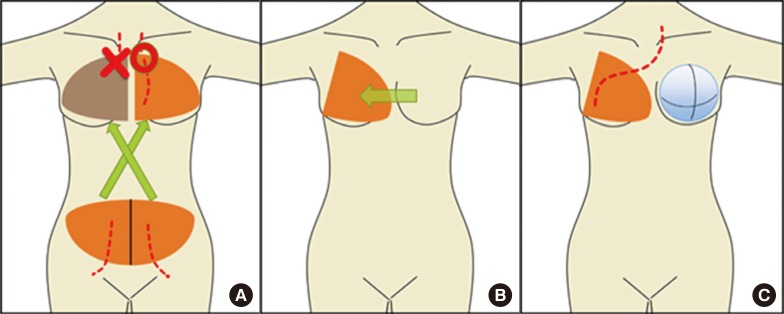
A 46-year-old woman underwent bilateral mastectomy for breast cancer. Axillary dissection, a skin graft from the abdomen, and postmastectomy radiotherapy were also performed on the right breast. We planned immediate secondary breast reconstruction with bilateral deep inferior epigastric artery perforator flaps. After elevating the flaps (Fig. 1), the vascular pedicle of the right flap was anastomosed to the left internal mammary vessels (IMVs) to reconstruct the left breast, and vice versa. However, after repeated arterial thrombosis, the flap on the right breast became unavailable due to intraflap thrombosis (Fig. 2A). Since engraftment of the flap was essential to accomplish the right breast reconstruction (due to skin insufficiency), and the ipsilateral thoracodorsal vessels were considered unreliable due to previous axillary node dissection, the flap anastomosed to the left IMVs was transferred to the right side through a subcutaneous tunnel (Fig. 2B). For reconstruction of the left breast, a tissue expander was placed under the pectoralis major muscle (Fig. 2C). Seven months later, the tissue expander was replaced with an implant (Fig. 3).
In the present case, we transferred a flap from the left breast to the right through a subcutaneous tunnel with the vascular pedicle connected to the left IMVs. The pedicle length (>10 cm) was enough to reach the contralateral breast without tension. Therefore, the use of IMVs on the contralateral side can be considered as an alternative option when the ipsilateral recipient vessels are not available [23], and flap pedicles should be harvested with the greatest length possible in preparation for such situations.